Will I find a job as a PA after COVID?
PANCE Points + QBank
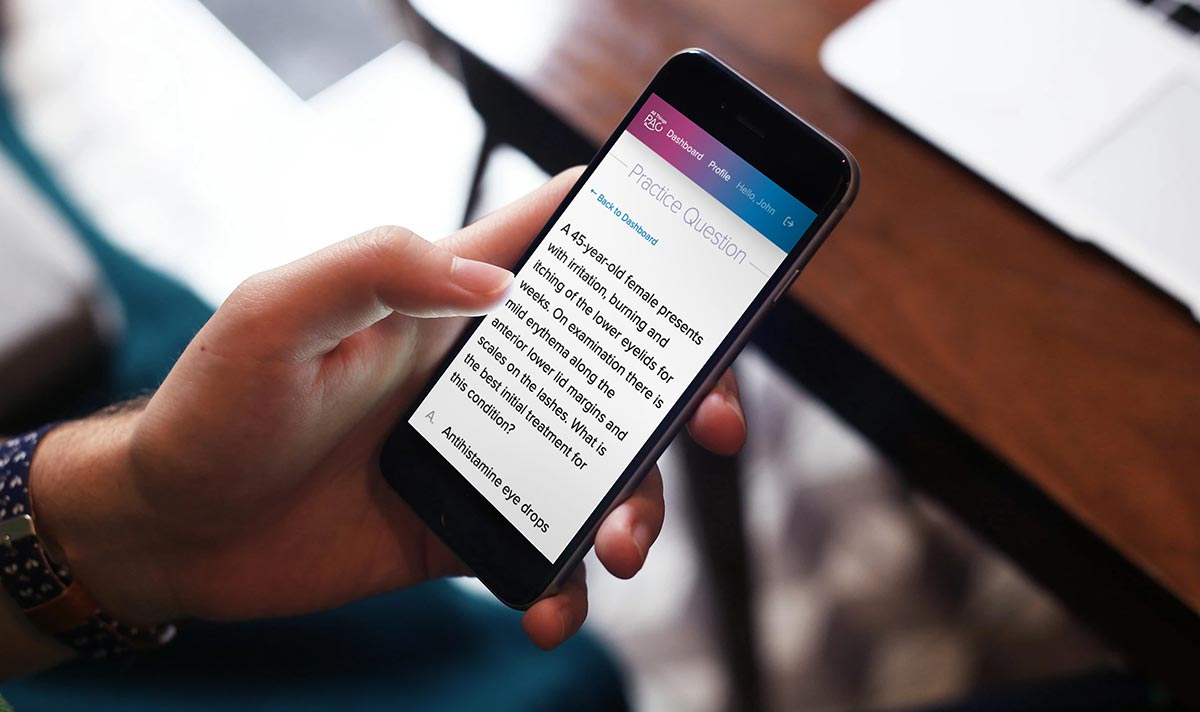
- 1,000+ questions written in the style & format of the PANCE exam
- Explanations for every answer to enhance learning
- Full-length practice tests following the PANCE blueprint
- Quizzes with choice of length & topic areas
- Individual practice questions with choice of topic areas
- Lifetime access
Six months ago, this question wouldn’t have even been on my radar. Healthcare jobs in general have been on the rise for decades, and PAs continue to hold one of the top positions in regards to job outlook.
But then COVID happened. And as horrible as it’s been to watch thousands lose their lives to this novel virus, including our healthcare colleagues, it’s also devastating to see the impact it’s had on PA and healthcare employment.
In April alone, healthcare employment declined by 1.4 million jobs. About 448,000 of those were physician and other healthcare offices. The feedback I’m receiving from PAs, new grads, and our community online is not great. Positions are being furloughed, hours and pay are getting cut, and hiring freezes are in place.
Here are a few comments I received on Instagram when I reached out about this topic:
ENT PA in Chicago… furloughed for 8 weeks. Hoping to get back ASAP!
Practicing NP in Texas, I work outpatient in internal medicine and patient numbers have dropped tremendously in the past few weeks but we’re hoping numbers increase soon as the stay home orders are lifted. NPs and PAs are very much needed and while most places are not hiring right now, they will in the coming months. Stay hopeful new grads and congratulations!
PA with 12 years experience and poor/ironic timing of contract ending. Everyone seems to be on a hiring freeze… (Including leads from months ago). I’m sure it will rebound, but uncertain how quickly.
New grad in Salt lake City Utah, applied to over 20 positions right around when this all started. I heard back from one of them, got an interview, and signed my contract last week. I imagine over the next month I’ll start hearing from all the other positions, but who knows. I’m just grateful I got a job so quickly after graduation. I still have very high hopes for our field!
I graduated last August, it took me six months to find a job and moving about 1,200 away from home ( I am from South Florida which is saturated with APPs). Then 3 months of credentialing, and just now finally getting my license which was taking longer than expected to process due to delays caused by Covid-19. I am now starting a few weeks after my expected start date, which is fine because things can still be worse. I have a job and look forward to learning as much as I can in order to grow as a PA. I think there will be jobs out there, but one is going to have to widen their search. To new grads, keep your head up and continue to push through this uncertain time.
I just graduated and have been searching for jobs for a while now. I had an interview and was in contact with a few places before COVID hit, but all hiring processes were put on hold. Trying to expand my interests for now to get a job, but I’m hopeful that more jobs will be available over the next few months
Emergency Med PA, hours cut to 8 hour shifts and company on a hiring freeze to ensure the current PAs and MDs get enough hours to reach base pay.
I’m in NYC, just graduated Friday. Under normal circumstances 3/4 of my class would have been contracted before graduation. Now it’s only about 1/4. I have been applying to orthopedic and surgical position. I am getting interviews and advancing to the last stages however I am getting told that the hospitals are on a hiring freeze and they’re doing all these virtual interviews proactively. They can’t tell me when they would be contacting about the job I am applying for. It’s very difficult and frustrating. I understand everything that’s happening and fortunately my family has not been affected. It’s definitely concerning as a new grad because once there is this “surge” are they going to be willing to train a new grad? Will I get the salary I would have prior to covid? Very anxiety ridden times
Graduated in March and have not seen many job opportunities in KY. Since COVID-19 I never saw any new job postings until now. And they are SLOWLY appearing.
Set to graduate from pa school in July in Pittsburgh, Pa. There are hiring freezes and the process is slow here too.
Derm PA in Ohio, been working for almost a year. Our office had to close temporarily, and I’ve been furloughed for 8 weeks so far. The more senior providers are back, but volumes are low and new safety protocols are still being perfected. I hope to get back to work this summer.
I’m in fam Med and I have had hours and pay reduced. It’s better than no job at all but wondering when it’ll get back to normal. There does seem to be more patients than during lock down but still low. It’s been about 1 month since the reduced schedule.
New grad in SoCal. Been STRUGGLING to find a single bite for jobs. Applied to well over 100. I have a possible urology job lined up but it’s a far drive. Better than nothing I guess?
New grad in Chicago. Began applying to jobs back in October before graduating and only once passing PANCE and getting my IL license did I start getting interviews, about February. Was in the midst of interviewing for 2 separate jobs in March when everything hit and all hiring was frozen. There have been basically no jobs being posted since mid March in Chicago.
These are only a few of the many comments I received.
For new PA grads, I know this has been a gut punch. It’s not what you had planned after graduating with thousands of dollars in student loan debt.
Most people agree at some point, volume will start to pick up again as we start seeing patients who have been put on hold for non-urgent visits and procedures. We may even see a surge.
We also know the physician shortage was present before COVID and will be present after. There is still a need for quality and affordable healthcare. PAs were and will continue to be part of the solution.
So what can you do now?
Remember why you’re here. You’ve worked this hard and your resilience will pay off. Don’t lose hope now.
Know your resources. Particularly when it comes to your student loans and how repayment is affected. Check out this link for student loan FAQs.
Be patient, but be willing to stretch yourself. You may need to consider locations and specialties that weren’t on your radar pre-COVID. In most cases, having a job is better than not having one. Not always, so make sure you know what’s best for you. But know you may have to settle for something that isn’t your dream job if you want employment. Just remember, nothing is permanent.
What do you do going forward?
Learn from our mistakes. What I mean here is don’t think PAs or healthcare jobs are invincible. I admit I did.
Save wisely for a rainy season such as this. I’m so thankful for having paid off my student loan debt early in my career. I don’t say that to brag, but I’m passionate about PAs having financial freedom from debt and today’s landscape is exactly why.
Consider having a second stream of income to make yourself more financially stable and versatile. PRN jobs and side gigs are great for this. Did you know the average millionaire has seven streams of income? When one goes away, there are plenty to fall back on. I’m not saying you need seven jobs, but consider having more than one stream of income, even if it’s small.
Lastly, trust yourself. If being a PA were easy, everyone would do it. It’s not easy to get here. You’re smart. You’re resourceful. You’ll get through this and figure it out. Just trust yourself.
If I can help or answer questions in any way, feel free to contact me at [email protected].
One of the most engaging topics of conversation I have with PA students has to do with the student loan burden of PA school. The average student loan debt for PA students upon graduation right now is $116,773. Many students have told me their debt is significantly higher. I believe PA school is a good financial investment. But I also encourage students to pay off their student loan debt as soon as possible. While I don’t claim to be the expert in this, I thought I might share how I paid off my PA school student loan debt.
I started PA school with zero debt. After undergrad, I got married and my husband and I made it a priority to pay off my student loans totaling around $10,000 (he had no loans). That number seems so small now, but at the time it was a big deal. We were newly married and had pretty low paying jobs.
We had both read Dave Ramsey’s book The Total Money Makeover and decided early in our marriage we wanted to strive to live without debt. If you’ve never heard of Dave Ramsey, I cannot recommend this book enough. It will literally change your life and potentially your family tree. Seriously, order it today! It’s a quick and easy read. I wish I could give it to every PA student!
Although the Dave Ramsey plan encourages you not to take out any loans, even for education, we decided PA school was something we were willing to invest in. I justified this knowing PAs make six figures and the demand for our profession is high with an upward trajectory. However, that doesn’t mean there are no risks. We probably all know someone who started medical or PA school, didn’t make it through, and was left with a mountain of debt and no degree.
I graduated PA school with about $85,000 in student loan debt. I know many of you have significantly higher debt. This was 8 years ago, so I’m sure at the time it was around the average. I was married and my husband worked while I was in school. He didn’t have a high paying job at the time, but his income certainly helped us not feel the stress of living loan check to loan check. We also had my first son seven months before I graduated. Those who’ve had children know they aren’t cheap. Between paying the hospital bills and childcare, money was very tight.
We also took out about a $5,000 personal loan from our bank when I graduated to cover moving expenses, take the PANCE, and have a little cushion before I started my job. That probably wasn’t necessary, but it helped us keep our bank account from getting closer to zero than I felt comfortable with.
So, total debt upon graduating: $90,000.
I finished school in August, passed the PANCE, and started my first job in the emergency department in late October. Oh, and remember what I said above about children being expensive? I found out I was pregnant again the day after I accepted the position. And for those trying to do the math, yes I was pregnant when my son was 8 months old. All that to say, life was getting expensive.
I remember my first paycheck came and it seemed a little surreal after making no income for almost three years. It was so much money to me. I think it was around $5,000. The next week our vehicle needed a new transmission which cost $3000. I thought, well, at least I’m making money now!
We reread the Total Money Makeover book to motivate us again, started following the plan, and began paying down our student loan debt. The only part of the plan we did not follow was I did invest in my retirement while paying off debt. Dave recommends you put that on hold in order to aggressively pay off debt, but I couldn’t turn down the company match. I already felt behind starting retirement savings at 27.
We did not buy new vehicles. I drove my 8-year-old Volkswagen Jetta to work and parked in the doctor’s lot next to vehicles that probably cost more than my student loans, and I did not care. My husband continued to drive our old SUV. We eventually “upgraded” my car to another SUV when I became pregnant with my third child.
We did not take big vacations. We did not purchase a new home. We had purchased a home during PA school and learned a lot of valuable lessons. Namely, don’t purchase a home until you’re financially ready or if you plan to move in the next few years. I knew whatever house we could afford now would not be the house we wanted to be in long term.
Dave Ramsey recommends your house payment not be more than 25% of your take-home pay. We decided not to purchase a home until our loan was paid off, and we could afford that ratio on a house we really wanted.
So, we rented a very small and inexpensive house. I live in the midwest where cost of living is relatively low and you get a lot of bang for your buck with real estate. Literally all of our friends were buying or building nice, large homes and we crammed into this cute little ranch on a half acre lot. When we moved out, our three children were all sharing a bedroom together. We did not care. We tried very hard not to compare our lives to others. And truthfully, I look back and have very fond memories of our first family home.
Because we didn’t have a large house payment, car loans, credit card debt, or any other debt, we were able to write large checks to the loan company. I would work a stretch of overtime then sit and write a $3,000 check to the loan company. I actually had to make myself not work as much as I could. I was very driven to pay off these loans but also knew I needed to be home with my family.
Even though we were making large payments, it felt very slow. Especially watching it all go to interest at first. After a little over two years, we had the debt down to about $45,000. I had actually hoped to make better progress.
But I realized we had two children during this time (which cost about $10,000 in hospital bills), as well as childcare for three kids (almost $2,000 a month). In addition, my husband wanted to try and work for himself, so we took a financial cut for a few months as he got his business off the ground. But we kept the end goal in mind and continued to inch forward.
When I returned to work after having my third child, it became apparent the ER life wasn’t working for us. Mind you my three children were all under the age of four. Working random night shifts, day shifts, evening shifts, long stretches on and long stretches off, was too difficult to manage. My husband would be home bottle-feeding the baby and bathing the other two, then attempting to put them all to bed before I would even get home for the day.
Around this time I received an offer to work in family medicine with a wonderful physician. But it would involve a $4/hour pay cut, plus no overtime or extra shifts available. This would surely slow us down even more from reaching our financial goals. But I knew it was the right thing for my family, so I made the move.
I know everything happens for a reason, and God wouldn’t ask me to make a move that wasn’t right for us, so I shouldn’t have been surprised to learn my office qualified for the National Health Service Corps (NHSC) loan repayment program. But I was.
I work in a town with a population of around 120,000, and a metro population about twice that. We’re not a huge city, but no one would call us rural. Apparently at that time, however, we did have a shortage of primary care providers. My site was a federally underserved area and qualified for the NHSC loan repayment.
There are many loan repayment programs, and I will eventually write a blog about these. In my opinion, most loan repayment programs are not worth it, especially if the contract is long. Many of them require you to work in rural areas where the pay is under average, and when you do the math over the duration of the contract, it doesn’t work in your favor.
This particular program however, is a good deal if the job is a good fit for you and you plan to stay. The contract is for two years of service in return for $50,000 in loan repayment funds. Now, be aware it is a contract. The financial penalties for breaking the contract are significant, more than the amount of forgiveness. You receive the funds on the front end of the deal.
For this program, you apply in March, find out if you’re accepted in July, and the checks are cut in October. I knew from other providers in the office I had a good chance of being accepted, so I started making only minimum payments on my student loans. You don’t get to keep the extra funds if your balance is under $50,000, which by this time mine was. By making only minimum payments, I could maximize how much of my loan was covered by the repayment funds.
I was accepted. One day in early October, a check from the government for $42,000 showed up in my bank account. It felt really nice to see that number in my account. But it was short-lived. The next day I paid off the remaining balance of my student loans. It was the biggest weight off of my shoulders.
Over the next several years, we bought our dream house, with land. I have no intention of ever moving. We upgraded our vehicles. We go on vacations. But honestly, we still have many of our same frugal spending habits.
We don’t have any type of payments or debt except our mortgage, and I don’t think we ever will. It’s funny, I thought once the loan was paid off we’d have all this extra money around. But I don’t know if that will ever be the case. We just reprioritize it. So now, instead of paying on the student loan, we save more in retirement and have college savings for our four kids (yep, I had one more!). When those are fully funded, we’ll probably do some work to upgrade our home. I don’t think we’ll ever have more money than we know what to do with. But we don’t worry about money. And as someone who grew up in a home where money was very tight, not feeling anxious or worrying about money is priceless.
I know some will say I really didn’t have it that hard. My loan was only $85,000 and the government paid a large chunk of it off. I would respond by saying, I get that. But $85,000 is still a significant number. And while I did receive the reimbursement funds, between my hourly pay cut and loss of overtime income, I made about $15,000 less per year in my family practice job than I did in the ER. So over two years, that’s $30,000 out of the $42,000 I received in reimbursement. I don’t think it would have changed our timeline much, but I’m very thankful it allowed me to have a more flexible job that fit my career and lifestyle goals.
I have no doubt if I hadn’t received the loan repayment, we would have stayed the course and continued to aggressively pay down the loan. Maybe it would have taken more than four years, maybe not. If my loan was $200,000, we still would have followed the same process, putting large purchases and goals on hold until we paid it off. We did it with $10,000 in undergraduate debt, and with $85,000 graduate school debt. Nothing would have changed.
I’m not saying this is what everyone should do. I will say once again, besides our careers, following Dave Ramsey’s plan has probably had the biggest financial impact on our lives. If you do nothing at all, just read the book.
If you still don’t see yourself being this aggressive about paying your loans off as quickly as possible, I at least challenge you to wait one year after graduating before making any major purchases like a car or home. Replenish your bank account and get a feel for what it’s like to pay your bills and see how much extra you can throw at your loans. Play with an online loan calculator and see how much money you save in interest by paying an extra $100 or $200 a month. Don’t increase the stress of educational debt by getting yourself into even more debt right away.
There you have it, my story of paying off my PA school student loans. I would love to hear yours!
UPDATE: This article was posted on 3/19/20. On 3/20/20, the ARC-PA issued a revised statement which can be found here. This speaks to the many students and programs who spoke out in support of PA students across the country during the uncertain times.
COVID-19, the quarantine, and all subsequent fallout has everyone struggling to figure out what to do next. Medical education is no exception.
As the CDC strengthened their recommendations on social distancing over the last two weeks, and while health systems combat PPE shortages and attempt to limit non-essential staff, nearly every PA program across the country is left scrambling to transition to virtual education. Didactic education is moving online and programs are trying to figure out what to do with clinical students pulled from sites.
While all PA students are anxious and worried about their education, one group in particular is left quite vulnerable. That is, those students expected to graduate this spring and early summer.
Let me start by saying, these steps have been necessary to slow down a global pandemic and prevent catastrophic consequences of this novel virus. I am not here to question whether or not PA students should be on rotations right now. I am in full support of social distancing and only using essential medical staff to limit exposure and preserve PPE equipment.
What I am here to talk about is the deplorable way both ARC-PA and some programs have handled this situation.
What Students are Saying
I asked my nearly 20,000 following of PA students and members of the PA community on Instagram, how their programs were handling this situation. Some said their programs are working diligently to figure things out and help them graduate on time. The majority, however, said they were essentially told “tough luck.” Reading through the responses broke my heart. I know many programs could be handling this better despite the ambiguous recommendations they’re receiving from ARC-PA, but I’m also not surprised because of how ARC-PA has responded.
ARC-PA’s Response
On March 10th, PAEA and ARC-PA released a joint statement attempting to guide programs as they respond and adapt during this pandemic. The statement was written when the primary discussion at that time was whether or not students should be potentially exposed to patients with COVID-19 symptoms while on rotations. They followed what AAMC was recommending for medical students at that time.
They also made the statement, “Please note that Waiving SCPE hours is not acceptable and if necessary, graduation time may need to be extended.” They then went on to say they were not planning on canceling their upcoming conferences.
And that was it. Today, March 19th, this is still the only statement they’ve released. My local gym has released more updates than ARC-PA. The problem is, our country has changed A LOT since March 10th.
Two weeks ago, we were telling students to limit their contact to suspected COVID-19 cases. Now, there are hardly any clinical sites even allowing students on site. We have new problems that need to be addressed by ARC-PA immediately in order for these highly intelligent and hardworking students to graduate in a time where we need healthcare workers in the field.
The Statement
Let’s talk about their statement. After bluntly telling us waiving any hours is not acceptable, they go on to say “Therefore, ARC-PA and PAEA encourage programs to contact the ARC-PA if their institutions anticipate significant changes in the program that may impact the structure, timing, duration, or location of the program. We encourage programs to work closely with their medical and community leaders to find effective ways to manage the education of students while maintaining compliance with the ARC-PA Standards.”
So, is there flexibility to make changes, or not? I reached out to ARC-PA on March 17th asking them to clarify what they mean by waving SCPE hours is not acceptable, but that programs can make significant changes to their structure and should reach out to ARC-PA if they do.
They responded the following day with “The ARC-PA has no further guidance beyond the joint ARC-PA/PAEA statement posted on our website.” By the way, as I type this, ARC-PA is still promoting upcoming conferences on the landing page of their website.
What Do the ARC-PA Standards Really Say?
So, if ARC-PA isn’t going to provide guidance, I will attempt to provide some. I am of course giving you my own interpretation of the ARC-PA standards based of my knowledge and some guidance I’ve received from mentors in PA education. Ultimately, what they say goes, and not my or anyone’s interpretation.
ARC-PA has standards for PA education that must be followed. Currently, they are using the 4th edition (a 5th edition will be utilized starting September 2020). PA programs are responsible for creating a program with competencies that meet these standards, and must be approved by ARC-PA.
In regards to SCPE (supervised clinical practice experience, or “clinical rotations”), the standards say this:
“Supervised clinical practice experiences must enable all students to meet the program’s learning outcomes expected of students, to include preventive, emergent, acute, and chronic patient encounters. Supervised clinical practice experiences must enable all students to meet the program’s learning outcomes expected of students, for patients seeking:
a) medical care across the life span to include, infants, children, adolescents, adults, and the elderly, b) women’s health (to include prenatal and gynecologic care), c) care for conditions requiring surgical management, including pre- operative, intra-operative,
post-operative care and d) care for behavioral and mental health conditions.”
It also says:
Supervised clinical practice experiences must occur in the following settings: outpatient, inpatient, emergency department, and operating room.
What is DOES NOT say, is how many hours are required in each clinical specialty.
A SCPE is essentially a course, just like any other course in the PA curriculum. Programs have the ability to set up courses however they feel is best. ARC-PA has to approve these when a program is accredited, but programs create their own SCPEs. Remember, ARC-PA only says SCPEs “must enable all students to meet the program’s learning outcomes expected of students“.
This means SCPES can include a variety of activities outside of direct, face-to-face clinical practice that help meet learning objective.
The problem we have now is that many programs set up their SCPEs, which were approved by ARC-PA, to only include clinical hours or number of patients. Those programs are feeling really stuck right now, because if their students didn’t meet that threshold, then there’s not much to do.
Side note to students: log every single patient you see on rotations. This is going to end up being a big deal. Yes, it’s annoying, but for some this is going to mean the difference between graduating on time or not.
Programs who structured SCPEs as more competency based, with flexibility for learning and assessment outside of face-to-face clinical hours, have more wiggle room here to figure out how students can still meet their ARC-PA approved SCPE rotation.
As it stands, it seems like many programs are in the former group.
Where Do We Go From Here?
No one is suggesting we lower the standards of PA education. But we all know there’s are other ways to learn and assess clinical competency outside of clerkships.
The feedback I’m getting is programs either don’t know whether or not they have flexibility, or they’re afraid to make changes for fear ARC-PA will say they are not meeting standards.
THIS IS WHERE ARC-PA NEEDS TO STEP IT UP AND SHOW THEY CARE!
ARC-PA should take notes from AAMC, who responded on March 17th stating they support medical students being pulled from clinical sites and will “organize efforts by our medical education community to compile and disseminate information and resources for alternative clinical learning approaches.”
They went on to do what ARC-PA certainly did not, and that was to reassure medical students by saying “We appreciate that this interruption and reorganization in student education raises concerns for students about timely graduation.”
ARC-PA, you need to support PA programs through this. You should be providing guidance on how programs can create alternative clinical learning experience in a time when we honestly don’t know when students will make it back to clinical rotations.
Everyone understands things are changing on the daily. You need to be proactive and malleable, like AAMC is. The domino effect of holding back students so close to graduation is a concern. What happens if we can’t get students back in rotations for three, four or five months? Where will we place current didactic students who by that time will also need clinical sites?
We’re simply asking you to do what everyone else has done, and that is pivot. Make creative and innovative adjustments. If you truly believe it’s not possible to do that while still maintaining high standards in PA education, then that says a lot about you and your limited beliefs in this profession.
Students, I Hear You
Students, I do hear you. And I am sorry. I’m so sorry your schools are not giving you information, or telling you they can’t do anything to help you. Ask your program what your SCPE competencies are and if there are ways to meet them outside of traditional clinical medicine. Push them for answers.
Programs. Do your part. Do your research. Look at your competencies and see if you have flexibility. ARC-PA said to contact them, so do that! Your students are scared and counting on you. Instead of telling them “I don’t know, you’ll have to contact financial aid,” why don’t YOU contact financial aid on behalf of all of your students? Advocate for them! Stay in contact with them!
I will continue to follow up on this. Word is, ARC-PA will soon make another statement. I’m not sure if that’s true, but hopefully it is. And hopefully they will follow suit with the AAMC and other medical professions who are finding alternative ways to work through this.
A petition is available for PA students who wish to express their frustration and charge ARC-PA with responding here.
I’ll be leaving the comments section open. Any suggestions or ideas to share for students, faculty and programs are welcomed.
I’ve debated back and forth on posting my opinion of the PA title change. Some days I care about it. But to be honest, most days I don’t. That is until the Title Change Survey came out last fall. We’ll get to that…
It’s not that I’m in love with our title; I loathe the word “assistant” just like the next PA. It’s a terrible title and doesn’t accurately reflect our education, level of autonomy, or clinical role. I want to poke my eyeballs out every time a well-meaning patient asks, “So when will you be a doctor?”
You can imagine the agony I experienced just 3 weeks ago when my 8-year-old asked me what PA actually stood for (I know, I’m not sure how I dropped the ball on that one), and after I answered he responded, “So you’re like a doctor’s assistant?”
That’s right… in my own home.
I’ve been a certified PA for almost 9 years. Early in my career, I would have been a staunch advocate for a title change. But the longer I’m in practice, the more confident I am and the less I really care about other’s opinions. I just want to treat my patients well and do my job. We can change our name to whatever we want, there will still be physicians and others who will only look at us as “not doctors.” There will always be patients who ask “So what exactly is a ____?” No title change will abolish that completely. It also feels like the public is becoming much more familiar with PAs and our scope of practice.
Because for years a title change was nothing more than wishful thinking, I simply moved on. But in July 2018, AAPA announced they were moving forward with a Title Change Investigation Advisory Council and designated an initial $1 million towards the project. Hello! So this is happening…
AAPA didn’t play around either. They hired WPP, the best of the best research and branding firms, to conduct the PA title change investigation. WPP was charged with answering the following:
- Is there a need to evolve the PA brand based on an objective, well-informed, data and analysis-driven view of where it stands today?
- And if so, how do we redefine how the PA profession is positioned, how its value is conveyed, and how it is titled to meet the requirements of tomorrow’s healthcare landscape?
WPP presented their initial findings at AAPA 2019 in Denver, Colorado last May and I was there to listen. And I have to say, I was impressed. Not necessarily with the findings (shocker, they determined we have a bad title). But I was impressed with the research. I was impressed with the researchers and the presentation. If AAPA was actually going to move forward with this, after all these years, I felt confident in how they were going about it.
I actually started to get excited about a title change and what this top tier company was going to come up with.
In November, many PAs and PA students anxiously checked our inboxes for the PA Title Change Survey we were told was coming in hopes of getting a glimpse of some of the options.
Prior to opening the survey, I heard some buzz on social media about the options. It wasn’t good. I sat down one night to open mine.
Oy vey.
It was asked that we not publically discuss or post the four title change options. And since I’m a professional, I suppose I’m not going to do it here. You can probably Google it by this point and find them. To say I was disappointed was an understatement. In fact, disappointment was the least of my concerning emotions. I began to worry about my future because if some of these ended up being a finalist, I was going to have to find another career. It was that bad. Two of the names were made up words for crying out loud! One of them too closely sounds like female genitalia or an STI. Just no.
Maybe I needed an outside perspective. I asked my husband who works in advertising and marketing. Nope. He thought they were terrible, too. Literally anyone I asked thought they were terrible. I have still yet to find a single person who is happy about the options.
WPPs portfolio is impressive. They work with multi-million dollar brands and AAPA didn’t cut corners in this process. But, between the two of them, the mark was missed.
I was honestly angry about it for a while. The more I thought about the options, the angrier it made me. I was perfectly content not caring about our terrible name, but now I was invested and this was the return.
I’m aware this is just a survey to collect more information and the investigation is still ongoing. But the tone seems clear: these are the likely choices. Again, I could be wrong, and I hope I am. We will hear next from WPP at AAPA 2020 this Spring. Between now and then, legal counsel will attempt to identify any potential conflicts with these titles, and the financial implications of making a formal title change will be determined.
Because I have four kids, a career, friends, and a million other things that actually matter, I eventually stopped thinking about this title change nonsense and returned to my former attitude of “I don’t really care what I’m called, I’m just going to do my job well.”
That is until AAPA released “Your Top Questions About the Title Change Survey Answered.”
The entire response was just so condescending.
“We recognize there were strong reactions to the names presented in the survey. This was expected. We read your comments on social media and on Huddle. We remained silent when the survey was in the field so as not to influence the responses. Now that it has closed, we want to address some of the questions and comments from PAs and PA students.”
This was followed by an unorganized attempt to politely say Thanks for taking the survey, we understand everyone hated all the choices, but we know what we’re doing here so just back off. Paraphrased of course.
They want us to know how extensive the process is. How hard it was to come up with names. That although we complained, none of us came up with any better names. (Side note, for $1 million I will come up with a great name. I’ll take a vacation and brainstorm something amazing while sipping fruity drinks on a private beach. You won’t be disappointed. Call me.)
Speaking of $1 million, they also mentioned we shouldn’t be complaining about the price tag of the investigation because it includes more than just coming up with four title options. So much scolding in one post.
My favorite response, however, was in regards to the made-up names which clearly drew a lot of negative feedback:
“There were invented titles for a reason. There is a reason “Verizon” became “Verizon” and not “Multinational Telecommunications Company” in order to distinguish itself in the marketplace.”
AAPA, can you hear me now? (see what I did there…) We are healthcare providers. We are professionals. Yes, PA is a brand, but we are not a phone company or a product. You cannot treat us as such. We’re already the red-headed stepchild of healthcare providers, can you please not make us the laughing stock of the entire industry?
I’m a member of AAPA. I feel a responsibility to support our profession. I like to think most of the people doing the work are really trying to do what’s best. But if you’re going to ask our opinion, please listen. Don’t send a condescending reply saying Thanks but no thanks, we actually didn’t really care what you thought.
You heard us. Now for the love, please come up with some better names.
Crossing my fingers, but not holding my breath, for the report coming out at AAPA 2020.

If you’ve followed me for long, you know practice tests are kind of my thing. And as much as I believe they’re one of the most effective study methods out there for PA students, I recommend utilizing multiple study methods during PA school. This includes study groups.
Study groups allow you to learn from each other and fill in personal knowledge gaps. They allow you to cover more material than one person can do alone. And a lot of research out there shows that studying in groups helps students learn more effectively.
One researcher found that certain dynamics of study groups contribute to learning in a way that studying alone might not. For example, his team identified the act of looking down to read your notes and thinking about what the instructor said, followed by looking up and explaining it in your own words to classmates, helps to learn the material on a deeper level. Eventually, study groups progress from looking down and reading notes to a free-flowing conversation about the material, demonstrating they have grasped the material.
Another study confirmed most students feel they learn more or different things when they study in a group compared to studying alone. This study also identified that it’s important to be working as a group, not in a group. Meaning, there needs to be a common effort, the utilization of the group’s competence, and the presence of problem solving and reflection.
I was one of those people who thought “I don’t study well in groups.” But PA school was the most challenging academic undertaking I had ever experienced. So I was willing to try anything that might be helpful.
After giving it a try, I can say I never left a study group wishing I hadn’t gone. Solo study remained my primary method of learning and retention, but I ALWAYS left group study sessions more prepared and confident in my knowledge than when I came. The key for me was finding the right people to study with and making the most of our study session.
So how do you make the most of a study group?
Here’s a few tips.
Keep your group small
Most experts recommend 4-6 people. Too many, and it can become an unfocused social event. Too few and you lose some of the benefits of a group study.
Hold your members accountable
Study groups should be a give and take. You learn from your classmates, but be prepared to contribute. It’s an environment where you deepen your understanding of the material, not show up expecting to learn everything from scratch. If someone consistently comes unprepared, lags behind in the discussion, or doesn’t contribute, it may be time to say goodbye.
Make the meetings regular
Regular meetings tend to be more consistent and productive. This could be meeting once a week, or perhaps you meet consistently 3 days before a big exam. But knowing you can rely consistently on a study group can be very helpful.
Create an agenda
Or at least a checklist of things you want to review. This helps you stay on track and know ahead of time what you can expect to cover. For those super Type-A groups, you can even assign each member different material to present to the group, make a study guide, or write practice questions. Put someone in charge of making sure the group stays on tasks and all material is covered.
Have fun with it
Yes, everyone needs to be focused. No, it’s not a social hour. But you can have fun with it. I studied with a small group of girls who all loved cooking (and let’s be honest, eating). Every once in a while we’d meet at one person’s house and cook a fun meal together, then study over dinner. Make quizzes or games to break up the monotony of reading through notes. As long as there’s a plan to stay productive, take the liberty to make the study environment your own.

This post contains affiliate links, which means if you click the link and purchase the item, I receive a small commission. All opinions are my own.
1) Gray’s Anatomy Women’s Mock wrap scrub top
These are my favorite go-to scrubs for comfort and style. They have a classic fit, plenty of pocket’s and they signature Grey’s anatomy fabric I love.
2) Grey’s Anatomy 6-Pocket Flat Front Pant for Women
These pants are nice fit you like a mid-rise pant with a flat front.
3) Littmann Cardiology IV stethoscope
My cardiology IV has lasted me 8 years and is still going strong. The double lumen tubing and durable quality make this one of the most popular stethoscopes on the market.
4) Dermlite
I didn’t know what I was missing out un until I used a dermatoscope in my family practice clinic. These completely change the game evaluating skin lesions, and now I don’t know what I’d do without one. Not just for derm, if you do skin exams at all I recommend investing in one of these for your office.
5) A Comprehensive Review for the Certification and Recertification Examination for Physician Assistants
Hands down the ONE review book I would have if I could only chose one. It goes through the entire PANCE Blueprint in a succinct but thorough book. Perfect to supplement your studies in PA school and guide you through board review after.
6) Yeti Tumbler
Because coffee is how I survived PA school and 12 hour shifts. This is the only one that keeps my coffee hot for hours.
7) Practice suture kit
It’s the next best thing to pigs feet (which are actually the closest resemblance to human skin I’ve found when it comes to practicing sutures). This is the perfect, less messy way to master your ties.
8) Travel case for your gear
Keep track of your gear with this cute and practical carrying cast that holds your essential medical equipment as you lug it from rotation to rotation.
9) H&P Notebook
This H&P notebook is perfect for students on rotations and PA’s that round on many patients. 100 H&P templates to write your notes now, staff with your preceptor and document electronically later. Perfect for keeping patient logs while on rotations, too.
10) When Breath Becomes Air
This New York Times Bestseller is one of the best books I’ve ever read (and I read a lot). This memoir from a young medical resident as he deals with a terminal cancer diagnosis should be a required read for anyone going into medicine.
I wrote 2 blog post this week about my medical mission trip to Greece last month. In Part 1 I discussed being the medical lead and all that went into planning a medical mission trip. In Part 2, I wrote about my personal experience on this particular trip.
Today in Part 3, I’ll answer the questions submitted through social media both during the trip and after I returned. My goal in sharing all of this is to hopefully inspire others to use their gifts and abilities to give back. That will look different for everyone and that’s ok. Big or small, your sacrifice is valuable to someone.
These questions are in no particular order.
1. How did you get involved?
A combination of looking for an opportunity and being asked to go. I had done a mission trip in the past and knew I’d eventually want to do more. I knew my church was considering putting together a medical team so I told them to keep me posted. I mentioned two organizations (GHO and PAGH) to check out if you are considering global missions, but honestly just start with your local community (your work or church) then go to Google.

2. What organization did you go with?
I helped plan this trip through my local church, but we worked with a church in Athens that has been well-established for years and has many ongoing community services to help the poor and needy in their community.
If you’re thinking about doing a medical mission trip, there’s rarely a reason to reinvent the wheel and plan something from the ground up. In fact, it can sometimes be harmful. It’s better to give local organizations the resources they need to provide sustainable services. If you’re considering a trip look for organizations that partner with local groups and resources in the area they serve.
3. What were you doing in Greece?
Greece has seen an overwhelming influx of refugees from Syria, Afghanistan and other parts of the Middle East over the last 10 years. Greece had nearly 20,000 new arrivals between September and October this year alone. It’s a crisis. These people left-there war-torn homes, cities destroyed, and have nowhere to go. When they arrive, there aren’t enough resources for them.
We were on the mainland in Athens (the situations are much worse on some of the Greek islands like Lesbos and Samos). We set up a small acute care clinic at a church that has been working to help some of the asylum seekers get integrated and established in the community.
4. Do other countries recognize PAs?
It depends. But this would likely only be an issue if you were only taking PAs, and no physicians. I know many PAs who have traveled to many different countries to serve, and they are typically under the umbrella of the physicians. Also, there are fewer regulations around humanitarian work than say, if you were moving to a country and getting a job.
5. Do organizations ever pay for your trip?
I’m sure somewhere there might be some that do. And there are some you can work for as a career. But for most, you are likely responsible to pay for it yourself. Many people chose to fundraise for trips like this. People who can’t (or won’t) go on trips still want to participate and feel invested in the cause when they donate. I had a few family members donate money for this trip, but I paid for most of it myself. However several of my team members raised all of the money through fundraising.
6. How much did it cost?
Our trip cost about $3,500 per person. This included airfare, room and board, food, medications, supplies, some group sightseeing activities, and a gift to the church who organizes the clinics. Several trips I looked at cost about the same.
7. What skills were you grateful for on the field?
I am good at counseling and patient education, and that is definitely a good skill to have. Being able to explain their problem in a way they understand, and what to expect or how they can take care of it with what resources they have, is of more value than medicine in many cases.
Other than that, really it’s the simple stuff. Laying hands on people, listening closely on the exam, and just knowing you don’t have a lot of tests and labs to help you out in many cases so get a good history and do a thorough exam.
8. What are the common illnesses you saw?
The same things we see here. Headaches, aches and pains, heartburn, upper respiratory infections, sore throats, skin issues. Very much like an urgent care. We did a little chronic disease management.
9. What was your favorite part of the trip?
Besides serving the patients, I really enjoyed meeting the other half of our team from Israel. They were a young group of translators and medical professionals we worked with and it was a lot of fun hanging out with people from a different culture. I went with a team from my town but a lot of people sign up for trips where they don’t know anyone. It can be a lot of fun to get to know other people this way.

Also, seeing Greece. I had never been and it was stunning. I was very careful to prepare my mind and heart that I was there to work and not on a vacation, but I am thankful I had time to see a new place. We traveled to Corinth on our last day. As a Christian, it was just a really neat experience for me to see the place where the Apostle Paul lived and preached and to think about the early Church in that place.



Corinth was amazing
10. How was it leaving your family for a period of time? How did you deal with the stress?
My husband is a rock star and a great dad, so I wasn’t really worried about anything. I did miss my kids dearly but Facetime makes it tolerable. When they are old enough, I would love to bring them along.
11. What tips would you give someone who wants to go on medical missions as a PA?
You don’t have much to lose by trying a short term trip. Start thinking about it a year ahead because it will take time to find one, catch the sign-up deadlines, save money, etc.
12. How does this improve your outlook/PA career?
I don’t think this does much for my resume or CV at this point in the game. Maybe it does. It’s definitely not a reason I do it though. The experience of doing it as a student though really made an impact on me.
13. What was the legal process (paperwork, documents) like?
Surprisingly minimal. I wrote about it in Part 1.
14. Have you always wanted to go on medical missions?
Yes. I live too good a life and make too much money (relative to most of the world) to not give back. Medical missions are the perfect fit. Not everyone is qualified to do it and the resources are needed.

15. How do you find trips?
Google. Ask colleagues. Check with large churches in your area. Check out GHO and PAGH. Finding a trip isn’t hard, deciding to go is.
16. How much free time did you guys have to explore and sightsee?
More than expected. The refugees prefer to get done early and get back home and back to the camps. We were done around 2-3 pm on most days. I don’t think that’s the case everywhere you go but it was for us. It was very nice and I greatly appreciate the time I had exploring the city, but if I go again I’d probably try to find a few other ways to be productive during the late afternoon. Perhaps other service opportunities in the city.
17. How do I get involved in a medical mission trip if I am still an undergraduate student?
Many trips take non-medical people to do things like triage, play with the kids, clothing/food banks, and many other activities. I’d look for trips and see if they offer positions for non-medical people. Let them know your interest in medicine and that might help!
18. What surprised you most on the trip?
It shouldn’t have surprised me, but I learned that we are all really more similar than we are different. Even if we come from completely opposite backgrounds or situations. We’re all just trying to do the best we can and care for ourselves and our families.
I was also extremely impressed with how a small little church in downtown Athens was able to do so many things for their community with moderate resources. It made me realize the potential we have to accomplish great things if we invest our time, energy and resources wisely.
19. Would you go again?
Heck yeah!
Hopefully, you read Part 1 of this series where I spoke about planning a medical mission trip. In this post, I will talk about my experience as a PA on this medical mission trip to Athens, Greece in October 2019.
Over the past 10 years, Greece has received over 50,000 refugees. Most of these were fleeing Syria and other war-torn areas of the Middle East. Despite being above capacity, Greece continues to see refugees cross their borders and arrive on shore daily.
Many of these will no longer be able to travel deeper into Europe. There is no easy answer for how a country, who wasn’t doing very well economically to begin with, will handle this crisis. But any success will likely start with helping these people integrate into what will most likely be their new home. This includes healthcare.
We arrived in Athens on a Saturday evening. The next morning, our team attended the church which hosts the clinic we came to serve in. It was a beautiful experience; doing something so familiar and sacred but with a different culture and in a foreign language.
We had headphones and an interpreter to listen to the sermon. The music was familiar songs, so we were able to sing the words in English along with the congregation singing in Greek. It was truly an unforgettable experience and reminds me a little of what Heaven might be like- those from all tribes and tongues worshiping together.


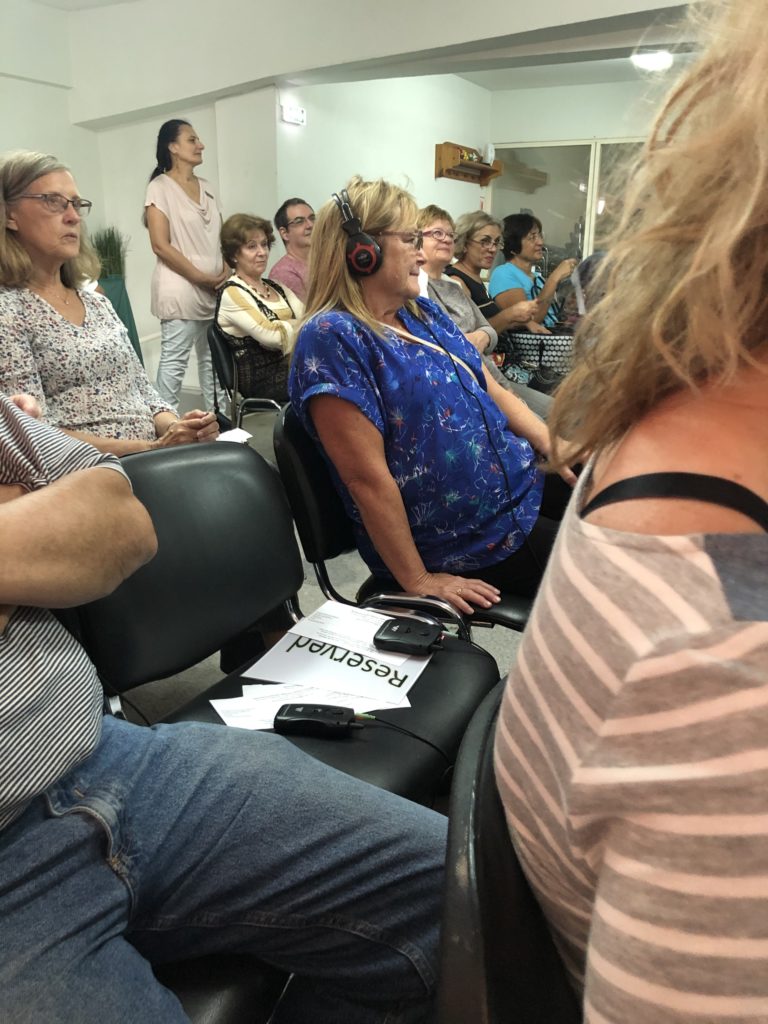

Sunday service
After the service, we unloaded our supplies and spent some time with the staff and volunteers there. They are a small church, about 100 members. But they do SO MANY things for their community. They have a food pantry, clothing pantry, English classes, and prison ministry just to name a few. They have specifically made an effort to provide services for the refugees and the poorest in their community.
Setting up
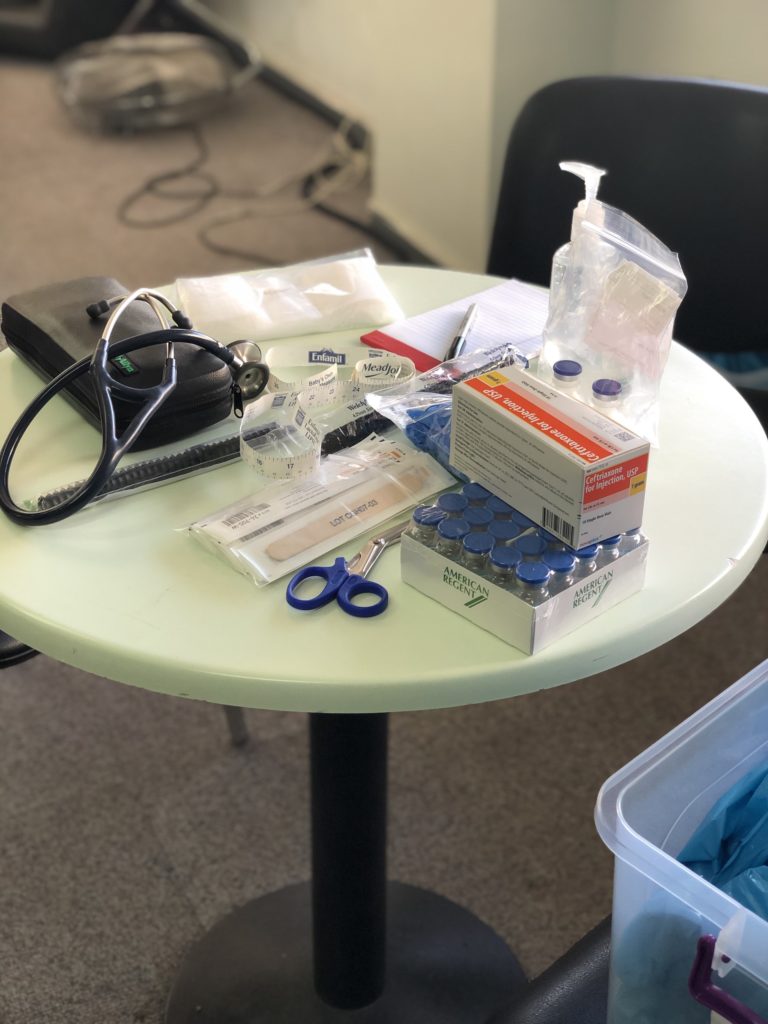
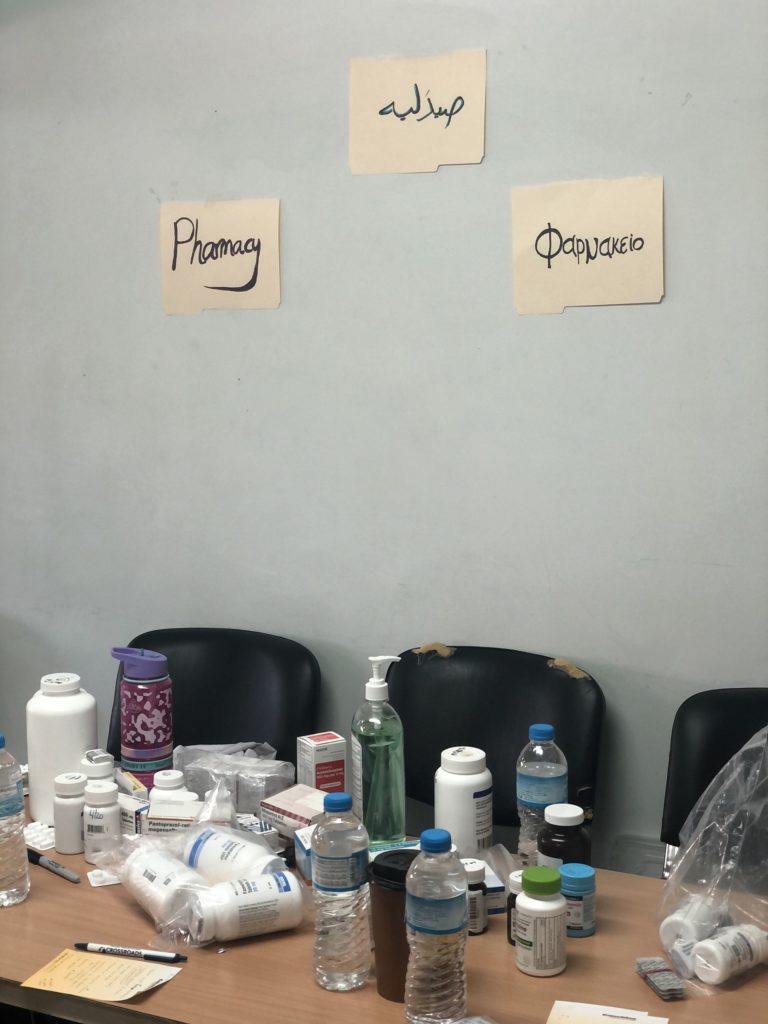
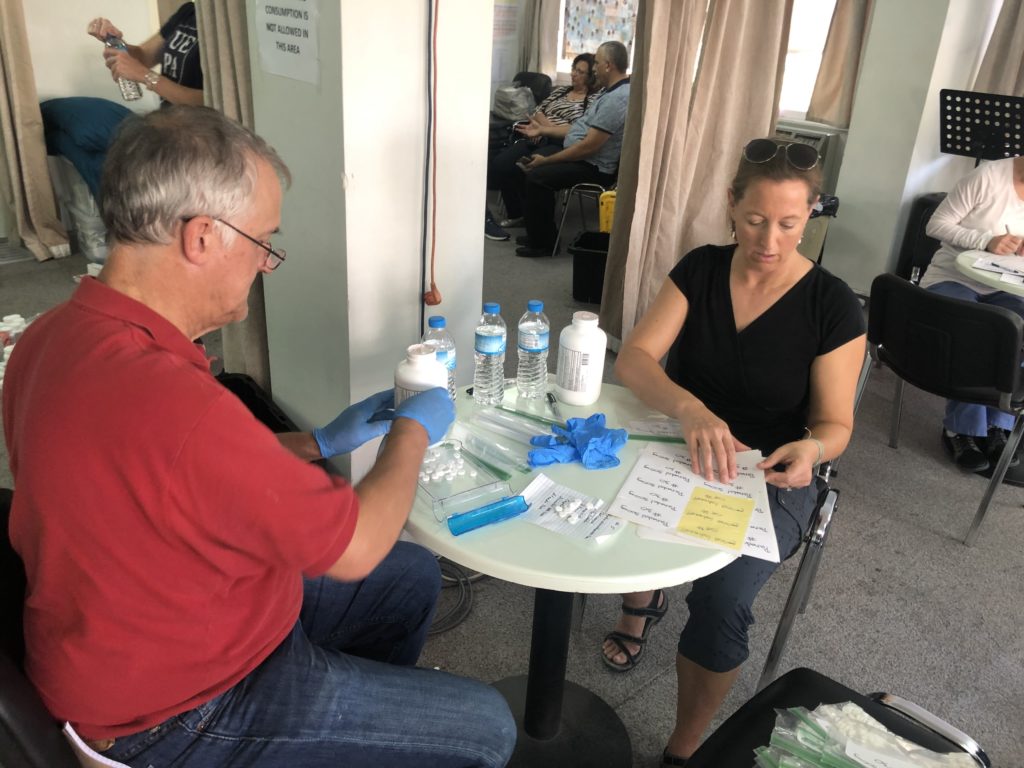
We took the entire next day to set up our “clinic.” I say clinic because it was really a large room we subdivided. My office was a small round table with my supplies and 4 chairs around it. Our triage was the small foyer of the church. Our pharmacy was a table in the corner, and our physical therapy clinic was a large corner of the room with a single exam bed. It was modest but mighty.
We counted and sorted pills for hours. This day we met our team of interpreters from Isreal. This was a young pharmacist, a family medicine resident physician, and two college students who spoke Arabic. All were a tremendous asset, but particularly we were fortunate to have two extra medical professionals. This team was so fun to hang out with, and we were immediate friends.

The next day, we arrived early and set up shop. The patients started arriving and our triage nurses handed out numbers and started intaking patients. The church attempts to keep some medical records for returning patients. We had simple SOAP notes we filled out, but nothing elaborate. It was a refreshing contrast from the exhausting documentation, time-stamps, and charting we have to do at home.
Our Patients
Patients of all ages and backgrounds came. Many mothers with their children, dads with children, entire families, and individuals. These are the cultures of large families. Their ailments were very similar to what I see here in the US- headaches, heartburn, aches and pains, and acute issues like fever, colds and sore throats.
But the etiologies were a little different. There were lots of headaches, but often these started when they left home months or years before. When I reviewed headache and migraine triggers such as fatigue, diet, stress, sunlight, etc… it was more like which trigger were they NOT experiencing on a daily basis?
Aches and pains? Weakness? Many of these people spent months traveling by land, sea, and air over long distances. Only to arrive somewhere to sleep on a hard floor, or crowded together, or on a bad mattress.
Weakness? I will never forget one young man with his small son, who when asked about why he might be weak, told our physical therapist he has no desire to eat or be active, because he is struck with grief over leaving his adult parents in Syria, and has no idea where they are or how they’re doing.
We had some, who weren’t actually sick but didn’t know when they’d be able to see a doctor or provider, so they brought everyone in to get “checked out.” Others brought labs, tests and office notes from local hospitals and asked us to look over them, and make sure we agreed they were receiving adequate treatment.
The Clinic
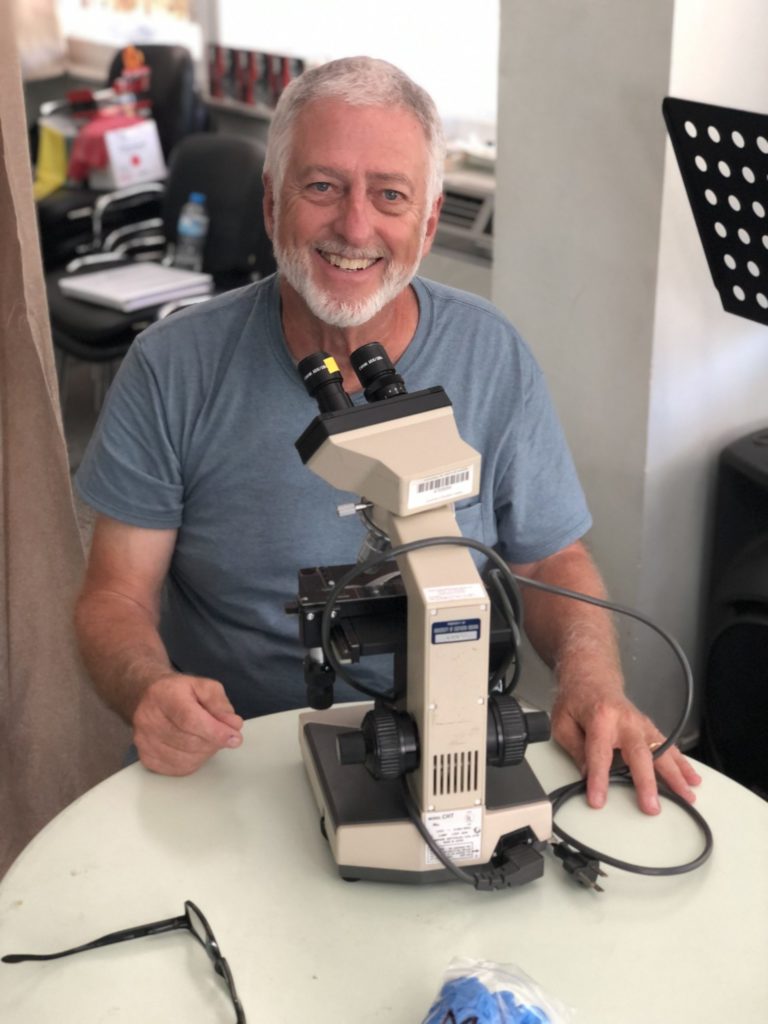
We didn’t have a lab, but we did have a microscope and a lab tech who was 78 years old and knew how to do manual slides. He actually taught me how to do this which was fun. Anemia. Everyone had anemia from poor diets and malnutrition. We tried to hand out iron supplements and vitamins to as many as we could.
What’s different about practicing medicine in a setting like this is without major resources we have at home, your history taking and exam skills become very important. You have to turn into sort of a MacGyver.
One young girl continued to have a recurrent ingrown toenail with cellulitis. Her mom begged us to remove the toenail. At first, I tried to apologize that we didn’t have the resources to dot that. But then I realized, maybe we do.
We had a laceration tray, lidocaine, some sterile drapes, and dressing materials as well as antibiotics. If we didn’t attempt this, she would surely continue to deal with this repeated issue.
The physician on our team and I arranged an exam table out of chairs and attempted through a translator to calm the young girl down. The digital block wasn’t fun, I’ll just say that. But she did great and we were able to do a partial nail removal successfully, bandage her up, and get her follow up care with the next clinic that was coming in a few weeks.
Visiting the Romani camp
We were asked by the pastor if we would like to spend one afternoon traveling to the Romani camp to provide medical care. The Romani people, often known by most as Gypsies (although this is actually a derogatory term), have a long and disturbing history of persecution. We were told the Romani camps in Greece were actually worse than the refugee camps. This church has been trying to build programs to help the Romani children receive an education and better integrate into the Greek culture, hopefully setting them up for a better future.
We traveled about 30 minutes outside of Athens to the camp. Upon arrival, I was struck with the contrast of the scene. If I looked in one direction, I could see the beautiful Mediterranean coastline. If I turned around, there were acres and acres of 3 and 4 walled structures, some with roofs and some without, and mountains of trash. No running water. No electricity. We went from 1st world to 3rd world in less than an hour.
Providing care was a bit of a mess. The kids came running first. Dirty, smelly, but smiles that made you forget that. Then the moms came. Not moms I was used to seeing. These moms were 14 and 15 years old in some cases. And with several kids. No men were to be found.
The Romani kids here get married very young (to young men as well). They have lots of kids early. They don’t receive an education. They never get ahead.
We were basically swarmed by the kids and moms, and tried as best as we could to provide care. There were lots of rashes and skin issues.
I remember seeing this during my trip to Mexico as well- when people saw others were given medication or really anything, others would come up and say they have the same problem even if they didn’t. They just wanted to be given something, anything. Even if it was just Tylenol and they didn’t need it.
We eventually got a little uncomfortable handing out medications we weren’t sure they actually needed and couldn’t confirm they understood directions on taking. Our translators here weren’t medically trained and a lot was getting lost in translation. The last thing I wanted was for a young mom to overdose her toddler with cough medicine. So we shut down our mini pharmacy and spent some time just hanging out with the people.
Again, this was just another experience where we were able to spend time and show respect to people who weren’t used to receiving that. On the ride back, the Pastor was sharing with me his vision to establish a program that would provide housing and education to Romani families who were willing to work and meet program guidelines. He is hoping to bring more medical clinics to the camp in the future, and he was glad to have us go and observe the environment. His vision for helping the poor and marginalized in his community, when the government, citizens and everyone else was turning a blind eye, was so inspiring.
My Takeaways
What I’ll remember the most about this trip is not providing medical care, but rather being able to look people in the eye who were just like me. They were moms, sisters, daughters, and friends. But because of things completely out of their control, they lost everything. And now found themselves in a new country, a new culture, and just trying to figure out the next step. People had stopped looking at them in the eye.
During one moment while my translator stepped away, I was with a woman my age and mom of 5 who brought one of her children in to be seen. Although I couldn’t speak to her, I put my hands on her baby and just smiled, saying her daughter was so pretty and sweet. I knew she understood me.
I then took out my phone and showed her pictures of my kids. She smiled and put her hand over her heart. I told her their names and she smiled some more. I knew that despite speaking different languages, we connected as two moms who loved their kids. Then, she reached in her purse and pulled out pictures of her children, pointing to them and telling me their names as a proud mom does. I smiled and told her they were beautiful but had trouble holding back tears. While I was showing her pictures of kids on my iPhone, she was showing me pictures from their asylum cards.
This woman was not very different from me. Born the same year. Smart. Driven. Probably even financially well off (most of the refugees who fled were ones who had resources and money and could afford to get out). Except unlike me, she lived in a country that would one day fall apart. And she would have no choice but to flee and try to protect her children. I will likely never know that kind of fear. These feelings were hard to process.
But what I can do, is not forget them. I can support trips like this by going, which I was so thankful to experience. I can support and fund organizations that are already established and making a difference.
I’m not speaking for anyone but myself, but as a physician assistant, I lead a comfortable life. I don’t have everything I’ve ever wanted, but I don’t want for much. I am grossly aware that is not how the majority of the world lives. This trip allowed me to see that first hand.
Again, speaking only for myself, I do feel a responsibility to give of my resources, be it financially or skills. I hope by sharing this, my experience maybe influences you to do the same. Not by guilt, but rather by inspiration.
And if that isn’t enough, it wasn’t all work. We had time for fun and a chance to experience beautiful Athens and even traveled to Corinth on our last day.
I ate some of the best food I’ve ever had that week. I was up close and personal to some of the world’s most historic landmarks. It was an amazing trip on all fronts and I hope to do it again soon.
In Part 3, I’ll do a Q&A style post about medical missions, answering questions you all submitted to me. Feel free to reach out or email me with any additional questions at [email protected].
I do not have many pictures to share of the refugees. Out of respect, and also for their safety, we were asked not to take photos. Many of them would receive persecution if it were known they sought help or care through a church or from Americans. I tried to post pictures I thought would be helpful to visualize the clinic and this experience.
I’ve been on two medical mission trips. I was a PA student the first time and traveled with one of our PA professors to a Mexico border city and provided primary care for the poor in that community. The second one was in October 2019, where I traveled with a small team to provide care to Syrian and Middle Eastern refugees settled in and around Athens, Greece.
The first trip I was a participant. I wasn’t involved in the planning, and because I was a student, I didn’t work independently. I basically signed up, paid for the trip, showed up with my passport, and went along. It was an amazing experience and definitely placed on my heart the desire to do a medical mission trip again.

What followed for me, as it does for many new PA grads, is a lot of “life.” New jobs. Moving. Babies. More babies (4 in total). Over the last 8 years since graduating, there hasn’t been a lot of opportunities to pick up and leave my family for 10 days. But now that some of my kids are self-sustaining (to a degree), and my husband and I are more established in our careers, these doors are opening.
All that to say there are seasons for everything, and if medical mission or relief work is something you want to do, it’s ok to wait for the right time.

For the Greece trip, I was the medical lead and in charge of planning the entire trip. If you know me, I’m not a detail-oriented person. I more of a big-picture kind of girl. A visionary if you will. So planning an international medical trip was WAY out of my comfort zone. As in, I didn’t know where to start.
How does a medical license work overseas? Is a PA recognized as a provider in Greece? Do we need malpractice insurance? How to you buy medications? How do you bring medications across borders?
I didn’t have a lot of resources and had to figure it out. But somehow It all came together. We took a team of 10; 1 physician, 2 PAs, a PT, 2 nurses, a lab tech, and 4 non-medical people across the world to extend care to those who needed it.
I received so many questions about how I was able to do this. Because there were so many, I’ll share my experience in two parts. I’ll speak more to the planning in this piece and more specifics about the actual trip in Part 2. Finally, I’ll post a summary Q&A post as part 3.
PLANNING THE TRIP
This particular trip was through my church. I’m a member of a nondenominational church of about 4,000, who sponsors several global mission trips yearly. They had not done a medical mission trip for some time, so I was approached about leading one. As I stated before, the timing felt right so I agreed. Especially since the cause was something that had been weighing on my heart for a long time.
Side note, I distinctly remember sitting in a lecture during PA school one day and reading about the new Arab Spring spreading across the Middle East (I know, I should have been paying attention to the lecture). For some reason, it stuck with me and I began to follow the tragic events that would take place in Syria over the next decade. But it all started back in PA school for me… little did I know I would eventually lead a medical trip related to this very issue.
Back to planning.
I was given a contact name of someone who had taken several US medical mission teams to Isreal, Jordan, Greece and Turkey where a large number of Syrian and Middle Eastern refugees have fled and settled over the last 10 years. If you’re not familiar with the Syrian refugee crisis, I recommend you read about it. It’s considered one of the worst humanitarian crises of our time. The city of Athens sees about 1000 refugees a week coming and they need resources, including medical care.
The previous groups my contact worked with were mostly through Global Health Outreach (GHO). I’ll stop here for a minute and make clear this is a Christian organization, and obviously going through my Church was part of a Christian mission as well. My church has two priorities when it comes to missions: Church planting among the least reached and social justice among the most vulnerable.
These issues are dear to my heart as well. My faith is a huge part of my life and one of the driving reasons for me to want to do missions. With that being said, my goal is 100% to serve and love people, not to promote an agenda.
So, if a faith-based organization is not your thing, there are MANY other opportunities out there. I would start by searching on the Physician Assistants for Global Health website.
Back to planning.
GHO had previously taken several teams to Greece so I was able to ask them a lot of questions about planning. But primary what I had to do was
- Build a team of medical and nonmedical professionals
- Determine the goals and objectives of the trip
- Make a budget and assist team members with fundraising strategies
- Lead my team in several formation meeting (a pre-trip meeting where we discuss objectives and prepare mentally and spiritually for the trip)
- Determine the necessary supplies and medications to bring
- Order said supplies and medications
- Determine necessary credentialing
Medications
In our case, we were aware of the number of patients we’d likely see in a day based on how many providers we were bringing, and what type of ailments they would have.
I used the formulary GHO had used and scaled it down to the number of patients my team would likely see. This was still a challenge- trying to figure out what medications to bring. Ultimately it was a large supply of over the counter analgesics, over the counter relief medications, steroid creams, antifungals, antihelmetics, and antibiotics.
We took a modest supply of chronic medications like antihypertensives and diabetes medications, but as you can imagine trying to manage these diseases at a short term acute clinic is not the best. But, we were able to fill some medications for people who were out.
I took a lot of notes while I was there on what we used and didn’t use. In retrospect, I wish we would have brought more acute medications such as cough and cold medicines. I also wish we would have brought enough iron supplements and vitamins to give everyone (we ran out around day 2). We had quite a few antibiotics leftover but packaged them up and left them for the next team. I did take a few vials of Rocephin and we used those for a one or two sick folks we saw. We took one laceration tray and a few procedure supplies, but not much. We ended up using them to do a toenail removal.
If you’re planning a trip and don’t know what to take, I would strongly suggest working with someone who has done a similar trip and using their formulary. Have your team look over it and make sure it’s medications they’re familiar and comfortable with. I also suggest connecting with a local pharmacist in that region. Some of the medications are much cheaper outside of the U.S. and you may be able to order or get supplies once you arrive.
Credentialing
The credentialing process was the most challenging for me. The reason being, there really wasn’t a process and I couldn’t wrap my mind around that. Long story short, people don’t really care about the poor and marginalized. At least in our case, traveling to Greece, there was no formal process to get approval to practice medicine.
We took copies of our licenses to have on hand. We had copies of the formulary and proof of purchase for the medications, and we had notarized letters from the church hosting the clinic stating we were coming to provide humanitarian relief. That was it. And we didn’t end up having to show it to anyone.
Insurance
Several people asked me about liability insurance. That was a concern of ours. I did some research and asked the previous teams who went and other groups who do short term humanitarian trips, and all agreed that malpractice insurance isn’t necessary.
Again, at the root of this, I think it’s because no one really cares about these people. Who cares if they receive bad care or have a bad outcome? I do think being from the U.S. we’re probably a little skewed on this topic because of how litigious our culture is when it comes to medicine.
I did end up finding a group that sells short term medical liability insurance for trips such as these, and to put the providers on my team at ease we purchased policies. They were dirt cheap, about $5 a day so I figured why not, you just never know.
Fundraising
I was fortunate to have someone helping me with logistics like travel arrangements, flights, hotels, so I didn’t have to manage that.
The entire trip costs about $3500 per person. Included in this were travel expenses, food expenses, medication and supply costs, a donation to the church in Athens that provides services and hosts the clinic, and a little to do some tourist activities. Our team had great success with fundraising a lot of this.
The primary source of fundraising was writing letters and personally reaching out to friends and family telling them about the trip. Many people will never hop on a plane, or maybe don’t have skills that are needed, to do something like this. But they still want to help with the cause. By giving money, they feel invested. We had some team members raise above and beyond this amount, which all went to support the medical clinic.

If you’re thinking about organizing a medical mission trip, I hope you find this helpful. It’s just skimming the surface but outlines the big tasks. I suggest that you not reinvent the wheel. Usually, people who have organized mission trips are happy to help. Find an established organization and build off what they’re already doing.
If you just want to go on a medical mission trip, and not organize one, then check out GHO or PAGH, or any number of organizations who are already in the trenches doing the work. Again, there’s no reason to reinvent the wheel and usually, these organizations are careful about who they partner with to provide quality and sustainable care where they go.
Lastly, understand you don’t have to fly halfway across the world to do this. I guarantee your local community has a need for low costs or free medical care. Perhaps there’s a low-income clinic that needs volunteer providers. Maybe you could start a program to provide medications or health education to those in need.
I do encourage you to find some way to give back. I don’t want to speak for everyone, but as a PA I don’t want for much. I have a decent income, a stable profession, and a wealth of knowledge. I feel that I have some responsibility to give back, and I hope others feel that way too.
Stay tuned for Part 2 where I will share more specifics about our experience in the clinic.

Students use numerous study techniques in hopes of absorbing a significant amount of information in a short period of time. Ideally, they retain this information for the long haul to apply clinically and practically in the real world.
But not all study techniques are created equal. One study looked at 10 commonly used study techniques. These included summarization, highlighting, keyword mnemonic, practice testing, imagery use for text learning, rereading, distributed practice, elaborative interrogation, self-explanation and interleaved practice.
They found practice testing and distributed practice were the most effective. Distributed practice, which is studying over multiple sessions instead of cramming everything in the night before, not surprisingly resulted in better long-term knowledge retention.
The study also found that practice testing with feedback is better than practice test alone.
Again, none of this sounds shocking but many students in PA school are hard-pressed for time and responsible for an exorbitant amount of information. That’s why one of my focuses with All Things PA-C is to provide practice test questions for students to incorporate in their studies.
So how do we create good, quality practice questions conducive to learning?
The PANCE and PANRE exams are multiple choice, so it obviously makes since that practice questions should be too.
Multiple choice questions can be used not only to test knowledge but to facilitate learning. One fascinating study showed how well-designed test questions enhanced recall of information. However, a poorly worded question can have the opposite effect.
Questions should be simple. Answer choices like “A and B but not C” are not as conducive to learning. You spend more energy trying to break down the question format than recalling correct information.
“All of the above” and “None of the above” are also not optimal. With “none of the above” you’re not recalling correct information.
Questions, as much as possible, should be “real world” centered. For example, knowing the difference between how two disease states would present might be asked “which symptom favors COPD versus heart failure?”
Or you’re given a symptoms and must come up with the diagnosis. “An elderly patient presents with progressively worsening shortness of breath and a pansystolic murmur. What is the most likely diagnosis?” Questions like this allow you to apply the knowledge in a real world setting.
Questions should offer a few responses that are reasonable choices with one being the “most correct.” Too many “close” answers make the question confusing and you’re not as likely to learn. As most questions on the PANCE have 5 answer choices, a format I like to use is one “most correct” choice, two plausible choices, one incorrect option, and one that is definitely wrong or potentially harmful. This can be especially helpful if you read the explanations behind why which answer is correct or incorrect. You glean as much from the wrong answers as you do the correct ones.
A test shouldn’t be too difficult. Answering too many questions incorrectly can increase the memory of wrong information. This doesn’t mean make the test easy, a test should judge how well takers know the material. If the majority of students miss a question, it’s probably a bad question. There’s an entire detailed process for determining the appropriate number of correct answers to pass the PANCE. And although no one that I know of would call the test easy, a large majority of first-time takers will pass.
Butler AC. Multiple-Choice Testing in Education: Are the Best Practices for Assessment Also Good for Learning? Journal of Applied Research in Memory and Cognition. 2018;7(3):323-331. doi:10.1016/j.jarmac.2018.07.002.
Dunlosky J, Rawson KA, Marsh EJ, Nathan MJ, Willingham DT. Improving Students’ Learning With Effective Learning Techniques. Psychological Science in the Public Interest. 2013;14(1):4-58. doi:10.1177/1529100612453266.