Six Figures Isn’t What It Used to Be: The Realities of PA Salaries in 2025
PANCE Points + QBank
- 1,500+ questions written in the style & format of the PANCE exam
- Explanations for every answer to enhance learning
- Full-length practice tests following the PANCE blueprint
- Quizzes with choice of length & topic areas
- Individual practice questions with choice of topic areas

Six figure PA salaries
If you’ve ever scrolled through PA school forums or watched “Day in the Life of a PA” videos, you’ve probably seen the same selling point pop up again and again: “PAs make six figures!”
And while that’s technically true, the average new graduate PA salary has risen from $98,412 in 2020 to $114,231 in 2024, the reality behind that number is more complex than it looks. Six figures doesn’t stretch as far as it used to, and what once felt like an upper-middle-class milestone now lands much closer to the middle of the pack.
A Changing Economic Landscape
Back in the early 2000s, a new graduate PA earned around $60,000–$70,000, which placed them solidly in the upper-middle-class bracket for many regions. At that time, home prices, rent, childcare and tuition costs were dramatically lower. That same salary, adjusted for inflation, would be roughly equivalent to $110,000–$120,000 today, meaning the buying power of a PA’s income has stayed nearly flat for 25 years.
Meanwhile, costs that hit new grads hardest like student loans, housing, and healthcare, have climbed much faster than general inflation. A PA starting out in 2025 might technically earn more than ever before, but they’re also stepping into a world where:
- Median rent in many metro areas exceeds $2,000/month
- PA program tuition can run well over $100,000–$130,000 for 27 months
- Loan interest rates have rebounded to pre-pandemic highs and are 2-3 percentage points higher than they were 20 years ago
- PA students 20 years ago borrowed less money and paid lower interest rates
- Home prices are up nearly 50% nationally since 2020
- Child care cost for full-time daycare averages $12,000–$18,000 per child, per year, with urban areas exceeding $20K
So even as salaries appear to rise, the margin of comfort has shrunk.
The Tuition Trap
Many prospective PA students still hear “six-figure salary” and assume it guarantees financial stability. But when paired with six-figure student debt, that equation changes quickly.
Let’s do some quick math:
- Tuition and living expenses: $120,000 total loan balance
- Average interest rate: ~7%
- Monthly payment on a 10-year plan: roughly $1,400/month
That’s before taxes, insurance, or retirement contributions, leaving many new grads with a tighter budget than expected, especially in high-cost areas.
What This Means for the Next Generation of PAs
None of this means becoming a PA isn’t worth it, far from it. The profession continues to offer strong job security, flexibility, and meaningful patient relationships. But it does mean that prospective students and new grads should approach the numbers with eyes wide open.
- Research tuition costs carefully. The difference between programs can exceed $60K.
- Consider cost of living when negotiating. A $100K offer in rural Texas stretches far more than $115K in Boston.
- Build a long-term financial plan early. Think beyond your first job and look at 5- and 10-year income trajectories.
- Advocate for fair compensation. As healthcare systems rely more heavily on PAs, our pay should reflect our value.
Final Thoughts
A six-figure salary is still an incredible achievement, but it’s no longer the automatic ticket to financial freedom it once was. For today’s PA students and new grads, success means pairing clinical excellence with financial literacy, strategic planning, and realistic expectations.
Preparing for the Physician Assistant National Certifying Exam (PANCE) can feel like a full-time job. Between lectures, rotations, and review guides, it’s hard to know what actually moves the needle on your score. That’s where a Qbank (question bank) comes in — giving you structured, interactive practice that mirrors the real exam.
Active Learning = Better Retention
Reading notes might help you recognize terms, but answering questions helps you remember them. Qbanks use active recall and spaced repetition to train your brain to retrieve information quickly — just like you’ll need to do on exam day.
Realistic Practice Reduces Test Anxiety
The PANCE is built on long, clinical vignettes with tricky distractors. Qbanks teach you how to analyze, eliminate, and reason through questions under timed pressure. The more familiar you are with PANCE-style questions, the calmer and faster you’ll be when it counts.
Instant Feedback Strengthens Weak Areas
Many Qbanks include performance analytics, letting you see exactly which topics (like cardiology or endocrine) need more attention. Instead of rereading entire review books, you can focus on the systems where your scores are lagging.
The Best PANCE Qbanks for 2025: Side-by-Side Comparison
There are several excellent PANCE Qbanks available — each with different strengths, question styles, and price points. Here’s how the top contenders stack up:
| Qbank | # of Questions | Key Features | Price |
|---|---|---|---|
| Rosh Review | 3,500+ | In-depth explanations, comparison to peers, mobile app | 💲💲💲 $199 for 90-day access; $319 for 180 days |
| UWorld PANCE | 2,000+ | Detailed explanations, visuals, difficulty similar to exam | 💲💲💲 $249 for 90-day access; $349 for 180 days |
| Smarty PANCE | 1,200+ | Flashcards, audio lectures, system-based quizzes | 💲💲 $75 for 90 days; $120 for 180 days |
| All Things PA-C Qbank | 1100+ | PANCE-blueprint aligned, concise rationales, includes PANCE Points high-yield review | 💲 $79 one-time access (lifetime) |
(Pricing as of October 2025 — subject to change)
Final Thoughts
No matter which Qbank you choose, consistency is the key. Even 10–15 questions a day can improve recall, reasoning, and test confidence. Combine question practice with focused review, and you’ll walk into your PANCE ready to crush it.
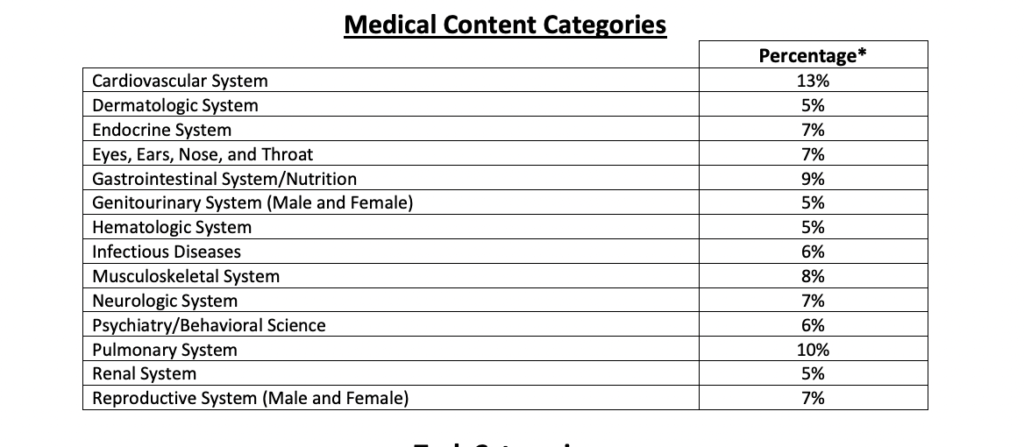
PA students are likely aware there is a new PANCE Blueprint that will take effect in 2025.
The National Commission on Certification of Physician Assistants (NCCPA) is the certifying organization for physician assistants. They are responsible for developing the Physician Assistant National Certifying Exam (PANCE). They also publish the PANCE Blueprint, which outlines the content and practice areas covered on the PANCE. PA students use the PANCE Blueprint to study and prepare for the exam.
Periodically, NCCPA conducts practice analysis studies to ensure the PANCE includes appropriate and updated content. The last update was in 2019. however a new PANCE Blueprint will take effect in 2025
What does this mean for PA students?
For those taking the exam in 2024, it means nothing. These PA students should feel comfortable using the 2019 Blueprint to study. PA students taking the exam in 2025 should use the new Blueprint. However, PA students adapting to the new PANCE Blueprint should not have much to worry about, as the changes are fairly inconsequential.
First of all, NCCPA has a disclaimer on the Blueprint that states there is no guarantee all topics will be included on the exam, and there may be some topics not on the Blueprint that are on the exam. PA students should remember the PANCE Blueprint is only a guide.
Secondly, in my review of the updated PANCE Blueprint, the changes are minor.
A look at the changes
The Blueprint designed to guide PA students preparing for the PANCE. The PANCE exam is categorized into two dimensions: knowledge of diseases an disorders and knowledge of skills related to physician assistant practice.
The Blueprint is also divided in two categories: medical content and task categories. The medical content category simply breaks down questions by body system. Task categories outline the skills tested.
The 2025 Blueprint, largely unchanged from 2019, is as follows:
| Medical Content Categories | Task Categories |
| Cardiovascular System | History Taking and Performing Physical Examination |
| Dermatologic System | Using Diagnostic and Laboratory Studies |
| Endocrine System | Formulating Most Likely Diagnosis |
| Eyes, Ears, Nose and Throat | Managing Patients |
| Gastrointestinal System/Nutrition | Health Maintenance, Patient Education, and Preventive Measures |
| Genitourinary System (male and female) | Clinical Intervention |
| Hematologic System | Pharmaceutical Therapeutics |
| Infectious Diseases | Applying Basic Scientific Concepts |
| Musculoskeletal System | Professional Practice |
| Neurologic System | |
| Psychiatry/Behavioral Science | |
| Pulmonary System | |
| Renal System | |
| Reproductive System (male and female) | |
| Professional practice |
New Categories
While the medical content and task categories remain largely unchanged, they did add professional practice as a medical content area and not just a task category like it was previously. Professional practice questions cover topics such as
- legal/medical ethics
- informatics
- patient care and communication
- the PA role in professional practice
- professional development
- public health
- risk management
Professional practice now makes up 6% of the exam instead of 5%.
Other changes include surgical topics now comprise 8-10% of questions (down from 20% in 2019) and 12-15% of questions will focus on pediatric patients (previously this percentage was not known).
Topic Changes
Minimal changes were made to the topics within the medical content categories. Most of these changes were really more of a reorganization of topics that were always covered on the exam.
For example, here’s a comparison of the topics that fall under Conduction disorders/arrhythmias:
| 2019 | 2025 |
| Atrial fibrillation/flutter | Atrial fibrillation |
| Atrioventricular block | Atrial flutter |
| Bundle Branch Block | Atrial tachycardia |
| Paroxysmal supraventricular tachycardia | Atrioventricular block |
| Premature beats | Bradycardia |
| Sick sinus syndrome | Bundle branch block |
| Torsades de pointes | Idioventricular rhythm |
| Ventricular fibrillation | Junctional rhythms |
| Ventricular tachycardia | Premature contractions |
| QT Prolongation | |
| Sick sinus syndrome | |
| Sinus arrhythmia | |
| Torsades de pointes | |
| Ventricular fibrillation | |
| Ventricular tachycardia |
The 2025 Blueprint is more specific as they’ve added more arrhythmias. But these added topics fall within the broad topics on the 2019 Blueprint, and exam takers were always responsible for knowing them.
Subcategory changes
Another change is recategorization of some topics and subtopics. For example shock used to be under hypotension, but is now its own category with specific types of shock listed.
| 2019 | 2025 |
| Hypotension | Shock |
| -Cardiogenic shock | -Cardiogenic |
| -Distruvtive | |
| -Hypovolemic | |
| -Obstructive |
Another example is coronary artery disease is now classified more consistently with how it’s managed in the clinical setting. In the new Blueprint STEMI, NSTEMI and angina all fall under acute coronary syndrome. Previously they fell under the subcategories of acute myocardial infarction and angina.
| 2019 | 2025 |
| Coronary artery disease | -Acute coronary syndrome |
| -Acute myocardial infarction | –Angina pectoris |
| –Non-ST-segment elevation | –Non-ST-semgent elevation myocardial infarction |
| –ST-segment elevation | –ST-segment elevation myocardial infarction |
| -Angina pectoris | –Unstable angina |
| –Prinzmetal variant | -Atherosclerosis |
| –Hypertensive emergencies | |
| –Secondary hypertension |
Take home message
Additional minor changes are noted throughout the new 2025 PANCE Blueprint. In the grand scheme of things, they are overall minor and should not significantly impact how PA students prepare for the PANCE.
Here at All Things PA-C, we are aligning our new study materials with the 2025 blueprint and will start going back to recategorized our Qbank with 2025 tags as well as the 2019.
Physician assistants must be licensed in any state where they practice medicine. If you’ve ever applied for a state license, you know the process can be long and tedious, taking weeks or even months.
A compact license is basically a way to avoid having to apply for multiple state licenses in order to practice in more than one state.
Think about it like applying to PA school. Most PA students used the CASPA application instead of filling out an application for every individual program they applied to. While applicants applying to multiple programs must meet individual program requirements, the process is streamlined into one central application. This makes sense because most programs are asking for the same information.
This makes sense for state licensure applications as well. Most states ask for the same information when granting a license, so why not have one unified application each state can use? Instead of taking weeks to get a license in a new state it may only take days.
This is a huge benefit for healthcare practitioners as things like telemedicine and locums work are growing exponentially.
A provider must have a license in the state where their patient is located. For example, I practice on a border state. While I live and practice in Indiana, I have a lot of patients who live in Kentucky and Illinois. But I can’t see them for telehealth visits unless they are physically in Indiana or I have a license where they are located at the time of their visit.
If you plan to work in telehealth, border states, or travel and locum jobs, this is going to be a game changer.
The PA Compact is not operational yet, but it is available for state legislative enactment. Currently AAPA is working to encourage states to join and more than a dozen have done so.
It’s estimated to take about 2 years for the compact to become operational.
Those just starting PA school will hopefully benefit from this advancement by the time they graduate.
You can follow updates on the PA licensure compact here.
In a world where information is at our fingertips, the realm of medical education is no exception to the digital revolution. Everything from learning the basics to keeping up with the latest medical advancements and guidelines has never been more accessible. Whether you’re a new PA student or seasoned physician assistant, podcasts have emerged as an invaluable source of knowledge.
Below are some of the best podcasts for physician assistant students recommended by both PAs and PA students.
1. Cram the PANCE

This was by far the most recommended podcast by PA students who submitted suggestions. The podcast covers all of the PANCE Blueprint topics providing tips and tricks to remember the massive amount of information needed to succeed in PA school and pass the PANCE. Check out the YouTube channel as well
2. PA in a Flash
This is another great podcast specifically for PA students. Host Courtney Shock uses an active-recall, flashcard-style review covering practice questions on PANCE and EOR topic lists.
3. Ninja Nerd
You’re likely familiar with Ninja Nerd’s YouTube channel where they break down physiology and medical topics for their 2.7 million subscribers with amazing whiteboard skills. Did you know creator Zach Murphy is a PA who hosts the Ninja Nerd podcast? If you love their YouTube channel, check out their podcast that focus on medical board content designed to help you pass exams.
4. The Curbsiders
Highly recommended and one of my personal favorites, Curbsiders is hosted by internal medicine physicians who interview experts on the subject matter covered. You’ll feel like you’ve mastered the topic after each episode. These episodes are fairly long, averaging about an hour, the hosts are entertaining and engaging. Great for commutes to and from school and clinical rotations.
5. The Cribsiders
If you enjoy The Curbsiders, you’ll love the Cribsiders who cover pediatric topics in a similar format.
6. The Audio PANCE and PANRE
Most PA students are familiar with SmartyPANCE (if you aren’t, please check it out!). But did you know Stephen Pasquini also has a podcast? This is another great review of PANCE Blueprint topics with episodes lasting 20-30 minutes and covering 10 PANCE and PANRE review questions in each episode.The free series is limited to every other episode, but the complete series is available to SmartyPANCE subscribers. If you’re not already subscribed, use this link and code AllThingsPAC for 10% off.
7. PA Exam Review
Brian Wallace from Physician Assistant Exam Review, covers core medical knowledge in easily digestible 20-30 minute episodes. This is another great Podcast produced by a PA specifically for PA students.
8. Medgeeks

Medgeeks publishes short and sweet episodes with topics catering to primary care and internal medicine. The host breaks down complex topics, debunks myths, and helps you stay up to date in medicine. Their goal is to provide medical content to help clinicians get through school, boards, and to excel in clinical practice.
9. EMRA*Cast

Emergency Medicine Residents’ Association is the voice of emergency medicine physicians-in-training. While it was created “for residents, by residents,” this podcast is an excellent resource for PAs studying emergency medicine topics and cases, and should be a rotating podcast for PAs working in emergency medicine. I listened to this podcast religiously in my ER days.
10. EM Clerkship
EM Clerkship is designed to help medical students master their EM clerkship, but is perfect for PA students as well. It covers different chief complaints, critical diagnoses, and skills important for the Emergency Department.
11. EM Basic
This is another great podcast designed for students in ER clerkships, but the range of topics covered spans across other areas of medicine including critical, primary, general and heavy coverage of pediatric medicine.
This post contains affiliate links, which means if you click the link and purchase the item, I may receive a small commission. All opinions are my own.
A common question among physician assistant students and other health professional graduates is whether they should create a curriculum vitae (CV) or a resume. There’s confusion about the difference between the two, and when is one preferred over the other.
What is a CV?
A CV is a comprehensive outline of professional milestones and statistics, including education, certifications, skills, experience, publications, and awards. Consider it a continuous log of professional accomplishments. As the individual accumulates more professional achievements and accolades, the CV grows. A CV is not meant to be abbreviated and polished; it should include everything that is relevant.
How is a resume different than a CV?
A resume is an abbreviated version of a CV, highlighting primarily education, qualifications, and work experience. It is tailored to the job posting to highlight qualifications desired for that position. Job searchers will often update and modify their resume when applying for a new position, whereas a CV tends to be more static and focused on the individual, not a job position. CVs are customary in academia and research-based fields, which is why they are commonplace in medicine.
One reason for confusion is for a new graduate with little experience and few professional accomplishments, their resume and CV will look very similar. And for most entry level positions, it likely doesn’t matter which one you submit. With experience, they will start to look different. Future jobs may ask for a CV or specifically for a resume. If it’s unclear, you can always ask for clarification and have both available.
Resumes tend to be 1-2 pages in length even for seasoned applicants. CVs tend to be much longer depending on experience, accomplishments and accumulated accolades. The following table highlights some differences between the two.
| CV | Resume |
| Often many pages in length | Generally 1-2 pages May include objective |
| Static- generally is not customized for a job description | May be edited and tailored for individual job postings |
| Very detailed | Abbreviated facts regarding work history and sill related to the job |
| Generally includes: -Education -Training -Certifications and licensure -Experience -Research -Accomplishments -Professional memberships -Presentations -Published works -References | Generally includes: Header with contact information -Professional statement or objective -Education -Skills -Work history -Certifications |
It’s important to remember there are no hard, fast rules. While hiring managers are accustomed to standard practices and formats on CVs and resumes, customizing your application is always an option.
For example, a new graduate physician assistant with limited experience is not going to have a substantial CV. Attempts to create one may lead to a bloated document that actually makes it harder to hold the attention of the reader. Following a resume format where employers can quickly view pertinent facts and information may be the better option. However, it may still include presentations, published works, honors and awards that set you apart from your peers.
I also recommend new graduate PAs tailor their resume for the job description. If you’re applying for an orthopedic position, include information about your orthopedic clinical and skills towards the top of your resume, and customize your objective statement to reflect your desire to work in that specialty.
As you develop professionally, maintain an updated CV so it’s readily available not only for job applications but other opportunities such as speaking engagements or professional events. A resume can always be created from an updated CV.
Templates and Resources
AAPA offers a free, but basic template for student members available on their website.
My Perfect Resume is a resume building tool with hundreds of industry-specific templates as well as expert advice to help you develop a custom resume, CV and cover letter. You can test the resume builder for free, however you can’t download or print any templates without purchasing a subscription. For most resume building tools, prices are not published or easily identified unless you create a resume, and My Perfect Resume is no different. At the time of this writing, a 2-week full access trial is available for $2.95. After 14 days it will automatically renew at $23.95 every four weeks, and you can cancel at any time. An annual subscription is $71.40 up front and will auto-renew after 12 months if not cancelled.
While you certainly don’t need a paid service or template to create a resume, I have reviewed My Perfects’s Resume‘s templates and process and do feel the services has a lot of value. I was very impressed with the variety of templates they have and how professional but unique they all look. You don’t have to worry about formatting or aesthetics, it does the work for you. Out of multiple resume building sites, this is the one I liked the most.
It’s difficult for PA students to include all pertinent information unique to PA school while still looking clean and organized, and for some this may be a services worth purchasing. You can always do the 2-week trial, just make sure to cancel your subscription before it auto-renews. But you may consider investing in the year-long subscription. Most students start preparing their CV/resumes and cover letters during the clinical year and make many modification over the next 6-12 months while applying for jobs. The tools in this service make that process much less painful.
Other resume building resource are listed below. Some have some limited free functions. Most of the paid plans are similar to My Perfect Resume, which is simply my personal preference after reviewing others.
Interviews are a two way street. While you have to sell yourself and prove you’re the best candidate for the job, it’s also important to make sure the job is right for you. In Part 1 of this series, we reviewed questions commonly asked during interviews and what to expect. Once you make it through the standard and awkward interview questions, it’s time to ask your questions and find out if this is the job for you.
The most important thing is to consider beforehand what you want to know. There are so many aspects of a job besides the required clinical skills. At the end of the day you want to be very clear on the expectations of the position and make sure you see yourself succeeding there.
When it comes time to ask questions, consider the following subjects and related questions.
Training and Onboarding
The Primary difference between training and onboarding is training is specific to your job role while onboarding focuses on integration into the company. For example onboarding should familiarize you with the mission and vision of the company, employee culture, understanding the organizational leadership structure, etc.
As a new graduate, you’re probably most interested in the training. Most employers understand there is a slower learning curve for new graduates than experienced PAs. Some questions to consider asking are
- How long is the training period for new PAs here and what does that look like?
- What is considered a “full schedule” for a PA here and how long do you expect for them to get there?
- Do I get to work with different providers during my training period?
- How are performance evaluations done and how often do these occur?
Expectations
While you’re likely familiar with the general expectations of the PA in a given specialty, every employer is different. If all you have for reference is the clinical rotation you were on, or perhaps no reference at all, make sure you’re clear on what the role is. Consider asking
- What does an average day look like for the PA here?
- How do the physicians view the role of the PA and how do they utilize them?
- What kind of administrative tasks are expected and is there designated time for this? (some employers offer “admin hours” dedicated for paperwork and other administrative tasks)
- How often should I expect to stay over or have to finish work at home? Is this common or generally an exception?
- How does coverage work when providers are out of the office? (for yourself and your colleagues)
- What is the role of nursing and support staff?
- What is the process for handling patient calls, medication refills, etc?
- How are calls handled off-hours?
- What are the expectations if I feel like something is out of my scope or I have a question? Are physicians readily available for me to discuss patients if needed?
Culture
This might be your dream job as far as specialty, but nobody thrives in a toxic work environment. No job is perfect, but you want to sniff out any major red flags if possible. Consider asking
- How long do your PAs stay here on average and what have been primary reasons for leaving?
- How would you describe the work culture here?
- Do you feel like staff and providers appreciated each other?
Benefits
It’s often difficult to judge when to bring up salary and benefit questions if they haven’t come up yet. Sometimes these topics are handled entirely by the HR department and may not be introduced until after you’ve been offered a position, or the people interviewing you may not be able to answer.
You also don’t want to sound presumptuous or overconfident by asking about benefits too early in the process, before they’ve had a chance to evaluate your skills and qualifications. But it’s fair to ask at least some general questions at your initial interview and certainly if you’ve progressed through the interview process.
You have to be careful not to judge your compensation by salary alone. Bonuses, call pay, overtime, etc contribute to thousands of earned dollars every year. For example, my current take home pay is approximately 20K more than my base salary each year.
Some questions to consider are
- How are PAs paid here? (this is a very general way to ask and they will hopefully describe all potential income. If not, you may have to ask specifically if it is salary, hourly, based off productivity, a combination any of these, and if there are bonuses or any additional sources of income)
- If there is a productivity component, ask if they can provide you an example of what previous PAs have made on average under that model.
- For positions where overtime is popular (ER, urgent care, etc), how often is it available and what are the expectations for filling extra shifts beyond your approved hours?
- Several positions I’ve seen have promoted a sign on bonus. Is that something you offer? (it NEVER hurts to ask!)
- What is the etiquette around vacation and taking time off? How much notice is required? Is there an approval process? Is there seniority?
- Is CME offered and is this typically something I choose or am I expected to attend specific trainings?
- Are licensing fees, DEA, board fees, etc covered?
Additional Questions
Really think through what you want to know and don’t hesitate to ask. Some additional questions might be
- How well does this health system approach multidisciplinary care and what does that look like? (This is huge in primary care; What is the referral process to have your patient’s see specialist? What would it look like for me to consult a specialist on a patient of mine?)
- Is there anything you could see a PA doing in this practice which they currently are not? (think procedures or things within your scope you’d like to pursue)
- Are there any leadership roles for PAs in the organization?
You don’t have to ask all of these questions. You don’t have to ask questions just for the sake of asking or trying to impress them. At the end of the day an interview is a two way street. They choose you and you choose them. No job is perfect, but make sure the job role, expectations and benefits are clear.

That first PA job interview is always a little nerve-racking for PA students. The combination of inexperience along with the unpredictability of interview questions in general, creates a lot of anxiety. But preparation will help you show up as the best version of yourself. These PA job interview tips will help you feel confident and land that first physician assistant position.
This blog series comes in two parts. Part one focuses on preparing you and covering common interview questions. Dozens of PAs submitted questions asked during PA interviews, and those are covered here. Part 2 will focus on what question you should ask to make sure the job is the right fit for you. Interviews are always a two way street.
The Interview
Remember, landing an interview means you are qualified for the job. The biggest obstacle for new PA students is inexperience. The fact that they are interviewing you, means they are willing to accept this. So let that settle your nerves a bit. Show them you are worth hiring.
Who Interviews You?
This depends completely on the position and setup of the clinic or health system. Often, multiple people are involved. This includes office managers, other PA or NP providers, physicians, HR representatives, medical directors, etc. Each person brings a unique perspective, so it is important to present yourself as a well-rounded candidate. For example, while one person focuses on your clinical skills, another might prioritize your communication skills or personality.
For this reason, they will ask a variety of questions. These questions will fall under subcategories. You can not predict what questions will be asked, but it is helpful to practice responding to question from different categories.
Question Categories
Questions tend to fall under one of several general categories. These include
- Get to know you questions
- Personality questions
- “Out there” questions
- Skills and clinical questions
Get to know you questions
These questions are all but guaranteed. Which means you should consider them soft balls. Have a script prepared and ready to go. Use these questions to showcase your best features and things that are interesting about you. Show them you are someone they want to work with. Examples include
- Tell me about yourself.
- How would your friends describe you?
- What gets you up in the morning?
- Why do you want to work in this specialty?
- What are your career goals?
When you answer these questions, be honest. But do not be boring. Talk about where you are from, or describe your family, but also tell them something interesting about you they are unlikely to hear from someone else. Describe a hobby or project you completed. Share about a fun trip you went on. They key here is to connect with them on a human level.
Personality questions
The objective of these questions is to determine how well you interact with people and if you have the personality traits and people skills to succeed. Examples include
- How would your friends and family describe you?
- How do you handle conflict?
- What is your greatest strength?
- What is your greatest weakness?
- How would you describe your work ethic?
- What would you bring to the team?
- Tell me about a time you had to think outside the box.
- Tell me about a challenging situation and how you navigated it.
- What is something people misconstrue about you?
- What is the last book you read?
Out there questions
The purpose of these questions are also to learn more about your personality, but are asked in a more non-traditional form. They require you to think on your feet and often leave people stumbling. Examples include:
- “Would you rather” questions
- What animal would you be and why?
- If you were a vegetable, what would you be and why?
- If you were a kitchen appliance, what would you be and why?
The sky is really the limit on what they could ask. The trick is not to think about an animal or an appliance, rather think about traits you want them to know about you. One way to not stumble on these questions is to “think out loud.” For example, if asked about what kitchen appliance you are, you could say “Well, I am a hard worker and I am reliable, so I would probably say a dishwasher. You can count on me to be efficient and work hard. I also clean up pretty good.” Verbalizing your thoughts avoid awkward silence and serves the purpose of expressing attributes about yourself.
The point is it does not really matter what your answer is. Rather, it is what you are relaying about yourself. People often stumble through these questions trying to think of something creative. If you first think of the traits you want to express, then find a response that matches that, you will be fine.
Skills and Clinical Questions
These questions are to get an idea of how you will perform in this specific role, and where you stand regarding experience. Remember, they know your experience might be limited as a new grad but still granted you an opportunity to interview. Let your work ethic and willingness to learn shine through.
Additionally, there is a chance you may be asked about procedures, guidelines, or specific clinical scenarios. Think about your experience in this rotation. If you did not have an opportunity to rotate in this particular specialty, think of cases you saw or draw on everything you know about the specialty. Have a challenging case in mind to present if asked. Think of the top 5 things you saw on that specialty, and be prepared to talk through a very general workup of those diagnosis. They may not ask specific clinical questions, but you do not want to draw blanks if asked.
Examples include
- How would you handle an influx of patients?
- Why are you a good fit for this job?
- What is your experience in this specialty?
- What are your favorite patients to work up?
- How would you manage (insert case scenario or diagnosis)?
- What screenings would you recommend for a 60 year old male patient?
- What would nurses/other staff say about you?
- How comfortable are you with (insert procedure or task)?
- What are you comfortable and not comfortable doing?
Wrap it up
While part 2 of this blog series will focus on what questions you should ask (the last question will inevitably be “What questions do you have?”), I recommend ending an interview by asking “Are there any reservations you have about me?”
This allows you to address any concerns or questions about you not presented in your previous responses. But be careful what you ask for. Be prepared to respond. For example, if they are concerned about how you respond to clinical questions, tell them “As PAs we are trained broadly in multiple specialties. I know I have a lot to learn in regards to this specialty, but am confident once I am in a clinical position I will master the clinical skills and knowledge required to be successful here. ”
If they express concern about your experience, respond by stating you understand their concerns but that you are a hard worker, willing to learn, and are confident with time you will be a valuable team member.
Two priorities for every employer are that you will do a good job and that you are going to stick around. Turnover is extremely costly for employers. End the interview by expressing a desire for the job and relaying confidence you are a good fit for the long haul. Consider something like, “Thank you for this opportunity. This interview only solidified my desire to work here as a PA in (insert specialty). I am not looking for just any job, I want to work somewhere that is a good long term fit for me and where I know I will make a difference. I really feel like this would be a good fit. Thanks again for your time.”
Come back for Part 2: What to ask to make sure it is the right job for you.
There is no shortage of resources for PA students. The challenge is finding affordable resources that cover all your needs.
While needs change depending on where you are in PA school, there are a few resources I highly recommend for everyone. Some of them are FREE, and the others are what I consider to be the best bang for your buck.
Having too many resources and study materials can actually be overwhelming. While I believe there are many great products out there, and encourage PA students to use a variety of resources, the products I’m recommending in this post are sufficient to cover all your PANCE preparation needs even if you have nothing else other than your school notes and materials.
Free Resources
The NCCPA PANCE Blueprint and PAEA Blueprint and Topic List
These two outlines should guide your studying throughout PA school, primarily in the clinical year and beyond. I recommend printing a copy of the NCCPA Blueprint and keeping it readily available. I suggest printing each EOR Topic List before that rotation and reviewing it frequently. Bookmark these pages on your browser and pull them up while studying. These organizations tell you what they cover on their exams, so why not use it?
NCCPA’s Sample PANCE Questions
This 13-page document comes straight from the horse’s mouth. I would argue no resource gives more insight into the style and format of the PANCE than this document. Here NCCPA provides old test questions and critiques written by NCCPA test committee members. See why certain answers are correct and why others are incorrect. There are only a handful, but the point is well-made.
Affordable Resources
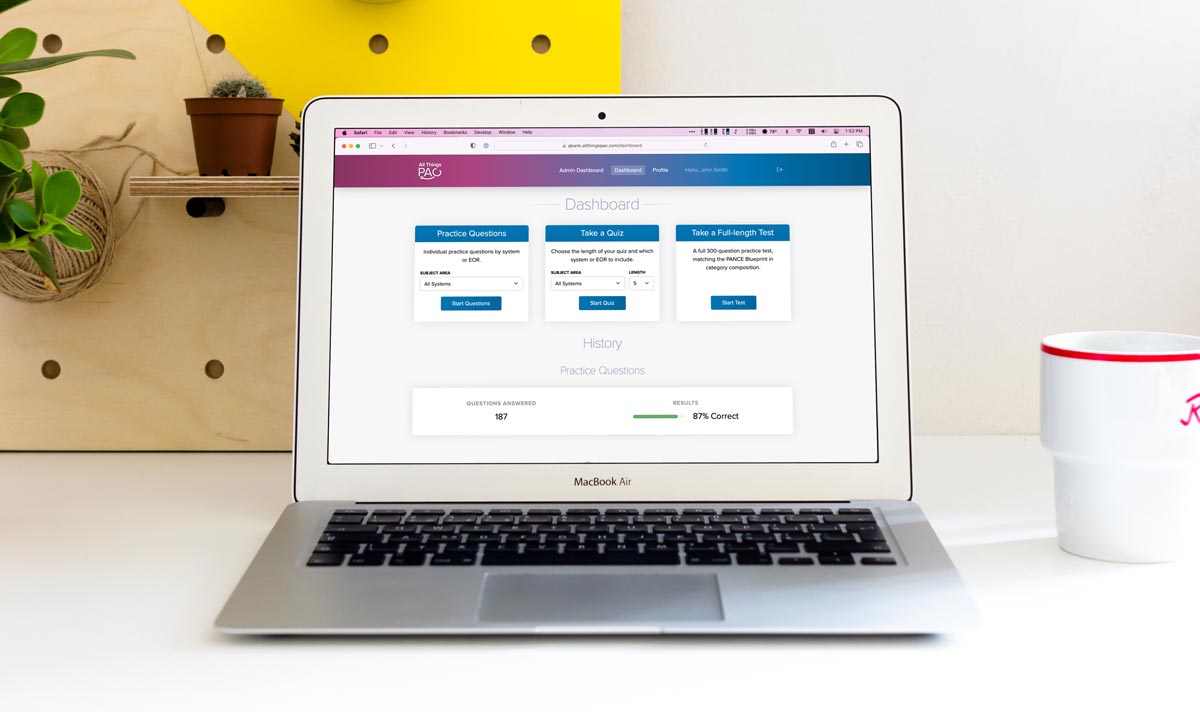
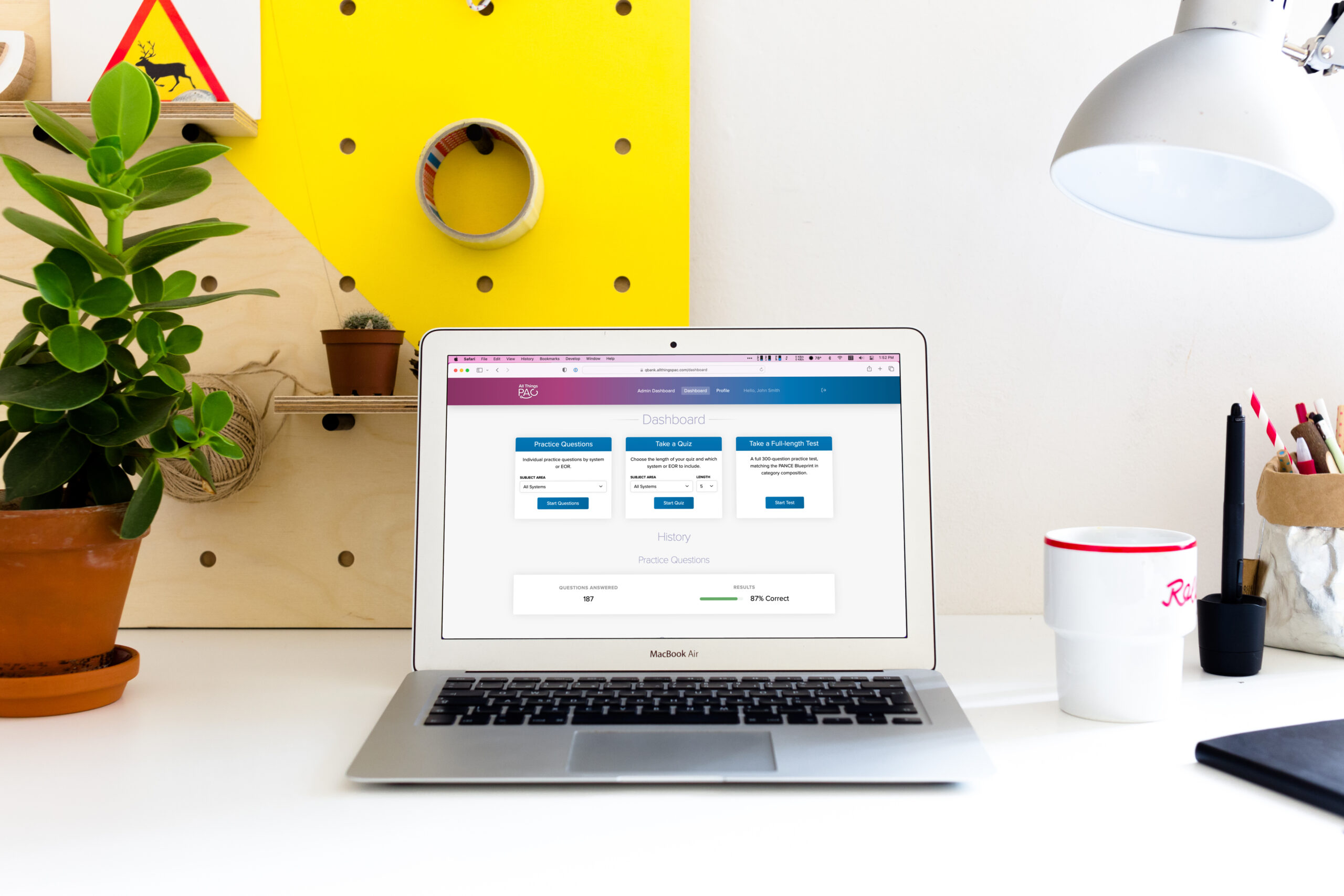
All Things PA-C Qbank
One of the reasons we developed the All Things PA-C Qbank was to fill a void. The goal was to provide a high-quality question bank at an affordable price point. Studies show practicing exam-style questions is one of the best study methods for passing board exams. Our questions are modeled using NCCPA’s style guide and closely resemble what you’ll see on the PANCE. Our Qbank allows you to practice questions developed using the NCCPA Blueprint, to filter by system or EOR subspecialty, and has the option to take quizzes or a full-length mock PANCE exam. Since launching in October 2022, at the time of this post users have answered over 118,000 questions and taken more than 2,500 tests and quizzes. One of the best features is, unlike other large question banks that are expensive AND require a yearly renewal, a subscription to the All Things PA-C Qbank comes with lifetime access.
Smarty PANCE
I have been recommending Smarty PANCE for years. Like myself, the creator is a PA who set out to make a useful and affordable resource for PA students. Besides our own product, it is the number one resource I recommend for PA students. A couple of reasons I love it so much is it follows the NCCPA and PAEA blueprints and includes succinct topic-focused reading material as well as practice questions. The content is concise yet covers all the most pertinent information on each topic. You can use it for a quick review or more in-depth studying if desired. It is also one of the best bargains out there as far as what you get for what you pay. I have a blog post with a full-review of Smarty PANCE that includes a discount code at the end you can use for 10% off.

A Comprehensive Review for the Certification and Recertification Examination for Physician Assistants
This is the resource I personally used the most when studying for the PANCE, and continue to purchase the newest edition to keep on my shelf. I used it for both the PANCE and my first PANRE. It follows the NCCPA blueprint and each chapter focuses on a body system and outlines in a concise, easy-to-read format everything you need to know. Each section has a few PANCE-style practice questions to assess your knowledge. Like Smarty PANCE, it’s a great resource to cover general information on every topic.
One of the missions of All Things PA-C is to provide free and affordable resources to PA students. At no extra cost to you, some of the products featured here contain affiliate links. This means if you click the link and purchase the item, I may receive a small commission. This does not influence what I recommend as all opinions are my own.
By the time PA students sit for the PANCE, they have answered thousands of test questions and logged hundreds of hours of board prep. Despite this, many leave the testing center feeling like the questions were different than expected.
The reason is writers of standardized tests use specific style guides to write their questions. The language, order of information, and other formatting is consistent for every question. A similar question asking for the same clinical answer, but written using a different style guide or no guide at all, will feel very different.
It is important for PA students to study for the PANCE using questions that follow the same formatting the PANCE uses. Test-takers need 100% of their brain power focused on analyzing the question at hand and identifying the correct answer. Energy spent trying to interpret confusing language or word order distracts the brain from the task at hand.
NCCPA formatting
I was fortunate enough to attend an NCCPA workshop several years ago. Their highly trained psychometricians discussed how the PANCE is developed – PAs and physicians from a variety of backgrounds are selected to write questions, and each question undergoes intense review by content experts and medical editors. Some questions identified to meet all standards then make it to the “pre-test” phase (the block of questions on the PANCE that is not scored).
After this, experts analyze questions to determine how well they perform and if they meet standards for inclusion as a scored-question on the PANCE. A question may run through the entire process only to be edited and submitted through the process again. Or it may get cut completely.
In addition to learning how the PANCE is designed, administered and its results interpreted, I was also given insight into the format and framework of PANCE questions and the general rules of thumb used in their style guide.
It has become the format we use at All Things PA-C when writing questions, and one of the reasons we receive consistent feedback about how similar our questions feel to PANCE questions.
The PANCE question framework
Second and third-order questions are most common
Test questions are categorized into first, second and third-order questions. First-order questions are straight forward. Second and third-order questions require additional steps and application to identify the correct answer.
An example of a first-order question is “Which medication has an adverse effect of hypotension?” A second-order question might say “A patient has shortness of breath, tachycardia, and hypoxia. He recently returned home on a transcontinental flight. Which test is considered the gold standard to confirm the suspected diagnosis?”
Most questions on the PANCE are second and third-order questions which require a deeper understanding of the application as well as how to apply knowledge of the subject.
Questions and answer choices will follow the same formatting
For most questions on the PANCE, there is a question stem, followed by five multiple choice options. One is the correct answer, and the other four are distractors.
The question stem includes a vignette and a lead in question. The vignette is the patient presentation, and the lead in question is what they ask you to figure out.
Every vignette on the PANCE will include the age, gender, site of care (clinic, hospital, ED, etc), presenting symptoms, and duration. This is almost without exception. If pertinent, the stem will also include personal or family history, vital signs, exam findings, and image/lab/study results. Questions will NOT include irrelevant information. If it is there, it is important. So pay attention to everything!
If the information is pertinent, it is included
Do not assume information if it is not given. An example is assuming an age, race or condition that is not provided, but leads you to choose one answer over another. For example, the question might ask “Which medication is the best first line therapy for a UTI?” The answer choices are trimethoprim-sulfamethoxazole, azithromycin, or amoxicillin. You choose amoxicillin because the patient could be pregnant, in which case you would not prescribe trimethoprim-sulfamethoxasole. However amoxicillin is not the best answer choice, the question never stated the patient was pregnant.
Everything you need to know to answer the question correctly is present. If you are relying on other details not given, you may miss the question.
There are no “made up” answer choices. You will not see non-existent disease names as a distracting answer choice.
Every distractor could potentially be correct, but only one can definitively be the answer. They are able to do this by stating “which one is the most” or “the best” choice. In addition, phrases like “of the following answer choices” defines that one of the answer choices is correct, although it is possible there is an unlisted choice that could also be correct.
Do not forget the details! Remember, vital signs are vital. Lab results are given for a reason. Often these details will help you distinguish between the correct answer and an almost correct distractor.
The answer choices on the PANCE are always in alphabetical order. While the question order is randomized, the answer choice order will always be the same.
Some questions you will not see
Exam writers are NOT trying to test what you DO NOT know.
You rarely, if ever anymore, see a negative question. Examples of negative questions are “Which of the following is NOT….” or “All of the following EXCEPT…” These questions are no longer used on the PANCE (but still exist abundantly in PANCE prep materials). In addition, there are no K-type questions. Examples of K-type questions include answer choices A, B, C, A & B, and A & C.
Go to the source
NCCPA is very open about how their tests are written. They have a PDF available of sample questions and explanations that explains why the correct answer is correct, and why the distractors are incorrect. Review this for an even better understanding of the PANCE format!
Our resources
Our resources and practice questions follow the same formatting and style guide used on the PANCE. Resources including an affordable comprehensive Qbank are available on our website.